WE ASKED TOP ENGINEERS, DOCTORS, EXPERTS AND INDUSTRY INSIDERS FOR NO-NONSENSE ANSWERS ABOUT WHERE PROGRESS STANDS ON SOME OF DENTISTRY’S BIGGEST CHALLENGES.
WHAT WOULD YOU WANT if you could ask for anything? How about half-price dental school tuition? Handpieces that last forever? Affordable robotics that lend a steady hand to any procedure? Scanners priced more like an intraoral camera? For Incisal Edge’s third annual Innovation Issue, we asked for hard questions, from practical to cutting-edge. Then we went straight to the most in-the-know people for their insights. To their credit, most were eager to participate.
Whenever possible, we let the responses speak for themselves, editing only for clarity. Many of these manufacturers distribute their products through this magazine’s publisher, Benco Dental, though that wasn’t a requirement for participation.
OUR METHODOLOGY
HOW DID WE arrive at these 21 questions? We started by polling a group of past Incisal Edge 40 Under 40 honorees and other friends of the magazine, a curious group of key opinion leaders we were sure would contribute thought-provoking questions and general guidance. (Spoiler alert: They did.) Special thanks to the doctors pictured below for their suggestions and, in some cases, ongoing participation during the production of this article. We weren’t able to address every idea, but one thought led to another, and not a single one went unconsidered. We’d also be remiss if we failed to acknowledge the considerable expertise of Incisal Edge’s publisher, Benco Dental, with more than 1,400 associates and a small army of experts who eat, sleep and breathe dental innovation, who were equally eager to contribute ideas. Thanks to all!
OUR THOUGHT LEADERS

Dr. Jaclyn Johnson
Kingwood, West Virginia

Dr. Jarod Johnson
Muscatine, Iowa

Dr. Sako Karakozian
Studio City, California

Dr. Jana Denzel
London, England

Dr. Michael T. Davey
Plattsburgh, New York

Dr. Gabriela Lagreca
Boston, Massachusetts

Dr. Adam Shinkawa
Fresno, California

Dr. Tu-Anh Vu
Brooklyn, New York
WHY NOT MORE ROBOTICS IN DENTISTRY?
Alon Mozes, CEO and cofounder of robotics company Neocis, says there are major differences between the way physician and dental robotics are developed, marketed, sold and used. Mozes would know; he was a principal engineer at an orthopedic robotics company before starting Neocis to develop Yomi, the first and only FDA-cleared robotic system available for dentistry.
 “First, the surgical approach is different, with surgeons using high forces for large joint replacement procedures, like hip and knee replacement,” Mozes (left) says. “Dentists tend to be much more delicate, with greater accuracy requirements. This changes the technology’s specification needs.” Then there’s the business side. “Medical device companies often have to sell to a small market of large hospitals with long lead times. Dental sales involve targeting a high volume of smaller practices, often owned privately by the clinician.” Finally, “there’s little overlap in the manufacturing. Many of the larger medical device companies don’t innovate in dental, and the large dental manufacturers are much smaller than the large medical manufacturers, leading to a gap in dental innovation.”
“First, the surgical approach is different, with surgeons using high forces for large joint replacement procedures, like hip and knee replacement,” Mozes (left) says. “Dentists tend to be much more delicate, with greater accuracy requirements. This changes the technology’s specification needs.” Then there’s the business side. “Medical device companies often have to sell to a small market of large hospitals with long lead times. Dental sales involve targeting a high volume of smaller practices, often owned privately by the clinician.” Finally, “there’s little overlap in the manufacturing. Many of the larger medical device companies don’t innovate in dental, and the large dental manufacturers are much smaller than the large medical manufacturers, leading to a gap in dental innovation.”
The perception that dental robotics trail in market penetration is not entirely accurate. There are hundreds of robotic surgery systems for physicians, Mozes says, yet “few have achieved a level of adoption that parallels what Yomi has. Yomi has been in development for more than 10 years and commercially available since 2017.” He says more than 130 practices nationwide have placed more than 23,000 implants with it. “Robotic dental surgery has crossed the chasm into mainstream use and will soon become the standard of care.”
He cites the cost difference between his Yomi unit and multimillion-dollar robotics for physician care, which are often accessible only by hospitals. Yomi, by contrast, “is affordable by both specialist and GP practices across the U.S.” As with all cutting-edge products, prices will likely fall in the coming years. Intriguingly, as they move beyond implants and expand to other procedures that require great skill and coordination, dental robotics “can potentially remove those challenges and level the playing field for
dentists of all experience levels.”
WHY NOT MATERIALS TO PREVENT, INSTEAD OF JUST TREAT, CRACKS?
Tooth fractures are the result of traumatic injury, which can occur via falls, collisions, biting down on hard foods and more. Structurally compromised teeth can fracture even under normal masticatory load. The etiology determines the location and extent of the fracture and, eventually, the treatment necessary.
Unfortunately, this means the only way to ‘prevent’ fractures is to avoid falls and eat only soft foods. What can be prevented, however, is a weakened tooth, which is more susceptible to fractures. Moderate and advanced caries and the large restorations that follow are preventable conditions that compromise tooth integrity.
In addition to maintaining good oral hygiene, managing early, non-cavitated carious lesions can help ‘prevent’ tooth fracture that may occur down the road due to the caries progression.
Curodont Repair Fluoride Plus by vVardis Switzerland enables one to do exactly this via in-depth Guided Enamel Remineralization. Noninvasive, drill-free, painless, non-staining, tasteless and requiring no anesthesia, this treatment can be provided by dentists and hygienists alike. Moreover, it’s especially beneficial in the pediatric population—who, as we know, tend to fall a lot.”
—Marzia Massignani, vice president, business innovation; and Dr. Divya Naik, oral health science liaison (EU) and prosthodontist, vVardis Switzerland
WHY NOT MORE DENTAL IMPLANT ATTACHMENT OPTIONS BEYOND SCREWS?
 It’s an interesting question, but sales figures show no slowing of demand for today’s implants. Steven Pfefer, a vice president at implant systems manufacturer Biotech Dental USA, tells us he thinks more clinicians are headed toward screw-retained prostheses. However, he notes there are “a few options where screws are not required”:
It’s an interesting question, but sales figures show no slowing of demand for today’s implants. Steven Pfefer, a vice president at implant systems manufacturer Biotech Dental USA, tells us he thinks more clinicians are headed toward screw-retained prostheses. However, he notes there are “a few options where screws are not required”:
- Abutments that have a morse taper fit. The components fit by a cold-weld seal. If you’re doing a full arch, it feels like natural dentition.
- Ball and Locator abutments can be used for restorations.
- Cementable abutments.
- Custom abutments with the crown luted onto the ti-base or custom abutment.
The bottom line: If you’re waiting for a revolutionary new attachment option that makes screws obsolete, it’s about as likely as a replacement for car tires that doesn’t use rubber or air. Today’s R&D time and money are spent on making screws safer, more predictable and easier to use—not on replacing them altogether.
WHY NOT OFFER A PRACTICE MANAGEMENT SOFTWARE OPTION FOR A STANDARD “DENTAL REPORT CARD”?
Only one of our panelists proposed this question, but it caught our attention. It seems useful to help patients track the progress of their treatment goals and plan. On the practice side, it might be a nifty tool to aid in treatment acceptance and perhaps “grade” how specific patients score relative to the overall patient population. Unsurprisingly, we couldn’t track down any existing software that currently incorporates a feature like this. However, Open Dental offers two interesting options for users who either have an idea for a new feature or the desire and wherewithal to create custom features for their own use:
From the time Open Dental entered the market in 2003, our product development efforts have been guided by our founder, a dentist, and by our dental practice customers. Open Dental’s Feature Request system allows practices to request additions or enhancements to the software that would be beneficial to their operations, and other practices can add their support for that feature and indicate if it’s critical to their process.
No customer has ever asked that we add a report card tool via Feature Request. However, Open Dental has an API [application programming interface] that allows a third party with expertise and a vision to create a new product, like a report card or risk analysis tool, and integrate it with Open Dental. Our open architecture allows practices to customize and integrate other specialized tools as needed to maximize the efficiency of their practice and serve the diverse needs of their patients.”
—Mark Johnson, vice president, business development, Open Dental
WHY NOT ANESTHETICS THAT ALREADY INCLUDE A BUFFERING AGENT?
 This has been frustrating dentists since the advent of local anesthesia in 1905. First, unfortunately, all local anesthetics do include a buffer, but that buffer is hydrochloric acid, which is what makes the anesthetic so acidic.
This has been frustrating dentists since the advent of local anesthesia in 1905. First, unfortunately, all local anesthetics do include a buffer, but that buffer is hydrochloric acid, which is what makes the anesthetic so acidic.
Acidity is necessary because the local anesthetic salts are weak bases and close to insoluble in water. In chemistry, if you have a weak base and you want it to go into solution, you buffer the solution with an acid, in this case HCl. Add to that the need for a vasoconstrictor like epinephrine, which oxidizes easily, and the anesthetic solution requires an even lower pH—so more HCl. The result of all this HCl is a solution that has the pH of lemon juice—the reason anesthetic stings on injection. Basically, when we inject, we create a wound and then bathe the wound in lemon juice.
Right now we need to buffer our local anesthetic, Onset by Onpharma, to a higher pH at the time of injection to create a more comfortable injection and relief from the acidity. There are other positives from raising the pH immediately before injection: less chance for failure, increased profundity and, most importantly, greater confidence in knowing that your patient is comfortably numb.”
—Dr. Mic Falkel, founder, Onpharma, and creator of the Onset Buffering System; assistant professor, local anesthesia, Arthur A. Dugoni School of Dentistry, University of the Pacific
WHY NOT A HANDPIECE WITH A “LIFETIME” TURBINE?
 TAKE 1: NSK
TAKE 1: NSK
Let’s start by clarifying that when we say lifetime, we mean something like the ceiling fan on your porch: long life, low maintenance and something you don’t have to think much about. A motor’s just a motor, right? But Keita Yokochi (right), handpiece guru for esteemed manufacturer NSK, says the difference starts with the highly consumable nature of ball bearings, which is compounded by extreme stress. “Ball bearings achieve extremely high speeds—400,000 revolutions per minute—to cut enamel, the hardest part of the human body, and other restorative materials smoothly,” Yokochi says. “This rotation speed is faster than a jet engine’s turbine and is probably the fastest rotation machine in any industry in the world. Such extreme high speed, massive abrasion and load during cutting imposed on those bearings and the entire turbine are continuous stresses during every treatment.”
Additionally, autoclaving handpieces, which exposes the bearings to hot steam, is mandatory. Those unavoidable elements may shorten the bearings’ lifespan. Yokochi likens handpieces more to a weather-beaten and road-weary car engine than to the easy life of your ceiling fan. “[A car engine] can last long but requires service and care,” he says. “Proper periodic maintenance can minimize stresses and may prolong its lifetime.” In other words, unless friction is somehow made to disappear, dental handpieces will always require maintenance and lubrication.
TAKE 2: DENTL EZ HANDPIECES by STAR
We also reached out to Star Handpieces, as it’s the only company we know that offers handpieces marketed as “LubeFree.”
Keep in mind that the ‘lifetime’ of a handpiece is relatively long compared to many consumer products—especially our Star handpieces. Some dentists will keep a handpiece for their entire 20-plus-year career.
The limiting factor on the lifetime of a turbine is mainly in the bearings and their support mechanism. The bearings in a handpiece are very small and spinning really fast. For comparison, the engine on a Formula 1 race car can run up to 20,000 RPM. Our dental handpiece is spinning 20 times faster—430,000 RPM. High speed generates heat, which eventually breaks down the bearing’s internal roller support, known as the bearing cage. When the cage breaks and the rollers aren’t supported, the rollers create even more heat and wear. This eventually prevents the turbine from spinning.
Lubricating the bearings can reduce friction and heat, but even lubricated bearings will succumb to the same failures as LubeFree. Over the years, Star has developed increasingly better bearings. We pioneered the use of ceramic rollers, which reduce friction, heat and wear. We’ve also developed numerous improvements on the bearing cage material that further reduce friction and maintain the longest life possible.
We understand the impact on a practice when a handpiece has to be taken out of rotation, even for a short time. Therefore, our turbines are field-replaceable, using the wrench and instruction supplied with the handpiece. They can easily be swapped out in a minute, which gets that handpiece back in action—fast.”
—Luther Gates, engineer, Star Handpieces
WHY NOT A SIMPLE METHODOLOGY FOR GPS TO DECIDE WHETHER TO TREAT AN ENDO CASE IN-HOUSE OR REFER TO AN ENDODONTIST?
 There is. Vatech doesn’t make a very big deal about it, simply calling it the “endo mode” in its Ez 3D-i CBCT software. While it’s not quite as simple as a computer telling users yes or no, the detailed images of canal shape, nerves, pulp structure and blood vessels—with accompanying color coding—make it easy to judge a case’s complexity and decide whether to proceed.
There is. Vatech doesn’t make a very big deal about it, simply calling it the “endo mode” in its Ez 3D-i CBCT software. While it’s not quite as simple as a computer telling users yes or no, the detailed images of canal shape, nerves, pulp structure and blood vessels—with accompanying color coding—make it easy to judge a case’s complexity and decide whether to proceed.
WHY NOT AN INEXPENSIVE DENTAL SCHOOL?
 Dental schools must prepare graduates to provide ethical and appropriate patient care immediately on graduation. A deep understanding of biomedical and dental science is necessary, a broad range of technical skills must be mastered and development of professional ethics must be ensured.
Dental schools must prepare graduates to provide ethical and appropriate patient care immediately on graduation. A deep understanding of biomedical and dental science is necessary, a broad range of technical skills must be mastered and development of professional ethics must be ensured.
All require the time and close attention of highly qualified faculty. Skilled clinical and administrative support staff are essential. Preclinical simulation and learning environments, clinical facilities and IT support must all be constantly upgraded. Faculty and staff must be paid competitively. Maintaining state-of-the-art facilities is expensive.
State licensing boards and the accreditation process provide external checks on outcome quality. Continued accreditation requires adequate resourcing, both human and financial.
Clinical revenue might contribute, but by their nature most predoctoral dental school clinics are break-even at best. Some states provide partial subsidy for the costs of education of in-state students in public universities, lowering tuition. Donors sometimes help. However, across the sector most of the financial resources necessary for quality outcomes must come from student tuition and fees.”
—Wyatt R. Hume, dean, School of Dentistry, University of Utah School of Medicine
Put It on TikTok: Perhaps in the future you’ll be able to use “ToothID” to unlock your phone. Dare to dream!

WHY NOT AN iPHONE APP FOR SHADE MATCHING?
TAKE 1: The Technologist’s View
 Shade measurement devices, including apps that work on an iPhone, are good for assessing flat, uniform color. Most devices are colorimeters that act like the human eye and measure red, green and blue. These are not accurate enough for dentistry. Spectrophotometers, which are pricier, are more accurate, measuring the entire visible light spectrum and applying a universal CIELAB notation that can be reproduced by applying XYZ values that represent value, chroma and hue—the science behind the VITA 3D-Master shade guide and VITA Easyshade.
Shade measurement devices, including apps that work on an iPhone, are good for assessing flat, uniform color. Most devices are colorimeters that act like the human eye and measure red, green and blue. These are not accurate enough for dentistry. Spectrophotometers, which are pricier, are more accurate, measuring the entire visible light spectrum and applying a universal CIELAB notation that can be reproduced by applying XYZ values that represent value, chroma and hue—the science behind the VITA 3D-Master shade guide and VITA Easyshade.
Most dental systems for color measurement recommend including a traditional shade tab in the photo. This effectively sets a white balance for the lab to refer to. But if the lab is going to use the shade tab shown in the photo, why use a digital shade-taking device? A closeup photo of the tooth is better to observe aspects the color device can’t see clearly, like characterization and surface texture.
Metamerism also plays a major role. Are the lips casting a shadow? Is the patient wearing lipstick or bright clothing? Is the light source color-corrected? These and myriad other ambient influences all affect shade measurement.
And while an intricate “shade map” can look great on a large computer screen, how do you reproduce this on a tooth the size of your pinky nail? It’s too much data! Lab techs generally prefer referencing their matching shade tab and the photos you sent.
Put simply: When a tooth presents curvature, reflectance, texture, translucency and metamerism, you find shade-taking apps on an iPhone to be inaccurate, since they just don’t account for these factors well enough.”
—Andy Klein, senior director, clinical education and events, Glidewell
TAKE 2: The Entrepreneur’s View
According to Dennis Braunston, the inventor of a technology called ShadeWave, the reason there aren’t five or 10 competing solutions is because “it’s not easy to develop a high-performing system that consistently meets the varying technical environments and needs of both dentists and laboratories.” Braunston says he and his team have invested more than 14,000 programming hours to arrive at their patented solution and adapt it into an easy-to-use iPhone app and desktop software they say is consistently accurate.
Given that its first customers signed on in 2014, why aren’t more dentists aware that ShadeWave exists? Braunston points to earlier attempts that were hardware-based and may have turned off potential users: “[That] approach is expensive, the products quickly go out of date and they don’t integrate seamlessly into the digital workflow.” So if you’re looking for a shade matching app, ShadeWave is a real option from a real company with real technology behind it.
WHY NOT A PRACTICE NERVE CENTER THAT CENTRALIZES SUPPLY AND STERILIZATION?
 While there’s no one-size-fits-all solution, there is an answer we call Office Nucleus. It isn’t just about safe sterilization or smart organization. Office Nucleus is designed to yield an intuitive system that imposes order and organization on these two vital areas of everyday care delivery. There’s one way in, one way out. Everything is placed precisely where you need it, eliminating frustration, wasted time and stress. It also slashes waste stemming from expired products. Most importantly, it’s designed to remain efficient and predictable for years to come, so owners can focus on patient care. That’s important, because practices can drift away from efficiency and adapt to chaos slowly without realizing it.
While there’s no one-size-fits-all solution, there is an answer we call Office Nucleus. It isn’t just about safe sterilization or smart organization. Office Nucleus is designed to yield an intuitive system that imposes order and organization on these two vital areas of everyday care delivery. There’s one way in, one way out. Everything is placed precisely where you need it, eliminating frustration, wasted time and stress. It also slashes waste stemming from expired products. Most importantly, it’s designed to remain efficient and predictable for years to come, so owners can focus on patient care. That’s important, because practices can drift away from efficiency and adapt to chaos slowly without realizing it.
To be frank, Office Nucleus is the product of decades of innovation, not something that we set out to invent. Benco Dental was the first dental distributor to offer customers space planning in 1978, and the first to launch automated supply procurement in 1988. We’ve been continuously improving both ever since. For instance, we started applying hospital best practices to dental office design during the pandemic, and added AI to our online ordering platform, shop.benco.com. We’d already been centralizing supply and sterilization for several years when we decided to formalize it as a set of standards, goals and principles that we can consistently apply to just about any design project. A successful Office Nucleus practice design is the sum of all that deep experience and those advanced tools. From design to installation to implementation, Office Nucleus is a custom and cohesive solution that quickly becomes second nature.”
—Taylor Haight, NCIDQ, project leader for Benco Dental’s Office Nucleus concept
WHY NOT MORE MOISTURE-TOLERANT RESTORATIVES?
 TAKE 1: PULPDENT
TAKE 1: PULPDENT
In his visionary article ‘Smart Materials in Dentistry,’ professor John McCabe teaches that most traditional dental materials are hydrophobic and are designed to have a relatively ‘neutral’ existence in the mouth. It is considered that if they are ‘passive’ and do not react with the oral environment, they will be more stable, have greater durability and cause neither harm nor injury. McCabe says this is an entirely negative approach and hides the possibility that positive gains can be achieved by using active—‘smart’—materials that behave in a more dynamic fashion.
It is a fundamental principle of science that biochemistry only occurs in the presence of water, and only materials that have the capacity to transport water have the potential for dynamic behavior. Only
moisture-friendly materials can release and recharge significant amounts of calcium, phosphate and fluoride to support apatite formation and the natural remineralization process. Traditional dental composites are hydrophobic and do not have this capacity.
Resins that stimulate remineralization of damaged tooth structure represent both the holy grail and the future of dental restorative materials. Pulpdent’s development of the phosphate-rich, hydrophilic Embrace WetBond resin chemistry was the innovation that allowed for the development of dynamic esthetic composites. In addition, Pulpdent overcame the brittleness of traditional composites by synthesizing a patented elastomeric resin molecule that provides fracture
resistance to the cured resin.
In 2013, Pulpdent added glass ionomer to these novel chemistries and introduced Activa Bioactive materials. This was a breakthrough that launched a new category of esthetic bioactive materials and a new conversation about the possibilities for ‘smart,’ esthetic, restorative materials for dentistry.
A true glass ionomer reaction requires a two-part material, and the next challenge was to create a one-part light cure bioactive material. Pulpdent synthesized and patented a novel methacrylate-functionalized calcium phosphate molecule with highly active remineralization properties. This is known as Crysta MCP technology and can be added to light cure or dual-cure materials. Crysta has been incorporated in Pulpdent’s Activa Presto stackable low-flow composite and Lime-Lite Enhanced light cure cavity liner.
These ‘smart’ materials play a dynamic role in the mouth and meet the challenge for moisture-friendly resin-based materials that are suitable for esthetic, durable, load-bearing applications.
Pulpdent is also making progress on bonding agents with mineralization potential and antibacterial properties that discourage MMPs and extend the life expectancy of composite restorations; bioactive CAD/CAM blocks; resorbable bone cements that stimulate remineralization and are replaced by natural hard tissue; orthodontic adhesives; packable composites; pulp capping agents; and other applications.
These innovations transition dentistry from a passive, reactive repair model intended to do no harm to an active approach using dynamic materials that support the natural remineralization process and preventive dental care that is better for our patients.”
—Fred Berk, vice president, Pulpdent
TAKE 2: 3M
According to Dr. Bradley D. Craig, senior division scientist in the Oral Care Solutions Division of 3M, hydrophilicity and hydrophobicity—the degree to which a surface attracts or repels water, respectively—is only one of many properties of the composite that are critical to its clinical performance.
“The mouth is a nasty environment for a material to survive, as it has to withstand mechanical forces, staining media, bacteria, pH shifts, solvents [ethanol] and wear from opposing dentition and food bolus,” Dr. Craig says. “It also must maintain esthetics and continue to function through all these challenges without things like swelling occurring. If the material is too hydrophilic, it will likely pull in moisture and swell—think of a dried sponge soaking up water. The methacrylate chemistry used in composites today tends to be fairly hydrophobic by nature, and the available monomers that are more hydrophilic have other drawbacks that make them unsuitable for a dental restoration. It’s obviously one of the industry’s ‘holy grails,’ and glass ionomers and resin-modified glass ionomers are probably the closest materials available that may fit the description. Unfortunately, those tend to have their own drawbacks and limitations, which have been well documented.”
WHY NOT A 3D INTRAORAL X-RAY?
Intraoral imaging has been limited to 2D until now, partly because 3D tomography requires space and time for allowing the sensor and the X-ray source to fully circumnavigate the head. This technique simply isn’t practical for the dimensions of a typical operatory. And because the sensor is located outside the oral cavity, the resolution is necessarily lower.
 Better intraoral imaging requires a different approach. The solution is to take a page from the established methods now used in mammography, which uses an imaging technique known as tomosynthesis. With tomosynthesis, X-rays are produced in a limited arc with no 360-degree view. Thanks to software reconstruction algorithms, a volume can be created from a multibeam focal array, then ‘sliced’ to show the inside of teeth.
Better intraoral imaging requires a different approach. The solution is to take a page from the established methods now used in mammography, which uses an imaging technique known as tomosynthesis. With tomosynthesis, X-rays are produced in a limited arc with no 360-degree view. Thanks to software reconstruction algorithms, a volume can be created from a multibeam focal array, then ‘sliced’ to show the inside of teeth.
As with 2D, the sensor is placed inside the mouth. This invention allows for a smaller device that fits into a normal operatory, using the same space and having the same form as traditional 2D intraoral imagers. While not strictly a 3D unit like in CBCT, the 3D Tomo method significantly increases the information relating to the pathologies inside the imaged teeth, allowing the dentist to ‘see’ more. It’s a cost-effective improvement in intraoral imaging.”
—Steve Andregg, vice president, Surround Medical, maker of the Portray X-ray system
WHY NOT AN AFFORDABLE DEVICE FOR MEASURING BITE FORCE?
 Somewhere between articulating paper and NASA-level technology is the Innobyte system from the Canadian firm Kube Innovation. It retails for $3,950 as of this writing, and it allows for accurate bite force measurements in seconds without extensive training required. Marianne Head, the company’s vice president of sales, says that users surveyed, on average, reported doing 24 percent more crowns and 41 percent more implant cases monthly. Viewed that way, it would seem to pay for itself relatively quickly.
Somewhere between articulating paper and NASA-level technology is the Innobyte system from the Canadian firm Kube Innovation. It retails for $3,950 as of this writing, and it allows for accurate bite force measurements in seconds without extensive training required. Marianne Head, the company’s vice president of sales, says that users surveyed, on average, reported doing 24 percent more crowns and 41 percent more implant cases monthly. Viewed that way, it would seem to pay for itself relatively quickly.
Similarly, users have reported that it’s helpful in explaining why crowns are a better option than fillings for certain patients by quantifying potential dietary limitations. “This is due to the fact that patients now better understand the need for treatment,” Head says. “They see their measurements correlated with easy-to-understand charts explaining how much force is needed to chew certain foods. Clinicians can also quantify the handicap that patients have to live with concerning their dietary habits and limitations.”
In the vast world of dental technology, $3,950 is a modest investment, but since there’s nothing comparable, we asked how the device landed at that price. Kube points to the costs of regulatory approval as one factor and, of course, the design of the product so it’s user-friendly and accurate. “That’s the main reason there was never such a device commercialized before,” Head says. She also notes that the cost of raw materials has exploded in the past year, with Kube now paying up to eight times the pre-pandemic amount for some electronic components. But the price could come down in the future, just as it has with intraoral cameras. “We see Innobyte technology being integrated into intraoral scanners. With this, we would simply need to produce the wireless AI-powered mouthpiece and not the full handheld unit. In the current form, we cannot lower the quality of our materials, as the requirements for medical devices are very strict.”
BUILD AMALGAM SEPARATORS INTO DENTAL VACUUM SYSTEMS AT THE FACTORY?
 The answer is more complicated than it might appear. Vacuum system manufacturers are capable of building the filter units themselves and offering them as an option with their products, which is done in Europe. However, it takes skill and considerable experience to successfully develop and produce effective filters. In addition, someone needs to process the filters. That’s a difficult ongoing responsibility, subject to regulation and significant liability, which involves the hazardous job of mercury disposal. It’s outside the focus and core mission of vacuum system manufacturers. This is where specialty companies like Solmetex, to name a prominent one, deliver value by creating specially developed solutions for efficient, cost-effective capture and disposal.”
The answer is more complicated than it might appear. Vacuum system manufacturers are capable of building the filter units themselves and offering them as an option with their products, which is done in Europe. However, it takes skill and considerable experience to successfully develop and produce effective filters. In addition, someone needs to process the filters. That’s a difficult ongoing responsibility, subject to regulation and significant liability, which involves the hazardous job of mercury disposal. It’s outside the focus and core mission of vacuum system manufacturers. This is where specialty companies like Solmetex, to name a prominent one, deliver value by creating specially developed solutions for efficient, cost-effective capture and disposal.”
—Paul Jackson, research consultant and former CMO of Benco Dental with more than 40 years of dental experience
WHY NOT A DSO-STYLE COMPANY TO HANDLE THE ADMINISTRATIVE DUTIES OF A PRACTICE, WITHOUT HAVING TO SELL?
Dental service organizations (DSOs) are an important component of the changing dental health care landscape. In order to succeed financially, they need to find synergies between the practices they own, such as reducing expenses and negotiating higher reimbursement fees.
“Own” is the key word in that sentence, because the changes necessary for those synergies usually require difficult decisions about people, partners and providers . . . decisions that are easier made as an owner than a service provider. For example, negotiating lower fees with a single dental laboratory for a network of offices is easy, but actually getting every office to use that single lab is difficult, especially if the offices aren’t owned by one entity.
So any company offering administrative support to individual dental practices without owning those practices (and therefore capturing the synergies of reduced expenses) will need to charge a hefty fee. Compounding the challenge: The firm will need to deliver those administrative services to individual locations over a vast geography (think: one office in Kansas, another in Georgia, a third in Oklahoma . . .). It’s a tough business model.

WHY NOT A MASK THAT’S TRULY BREATHABLE?
 If you’re pining for a mask that provides extreme protection with no breathing resistance, that’s a long way off. Richard Cohen, Benco Dental’s managing director, is our go-to guy when it comes to PPE; he has spent more time than anyone we know visiting factories worldwide and delving deep into R&D. “You can’t have ‘easy breathing’ and ‘tight filter’ in the same product,” he says. Gary Steinberg, president of Medicom North America, agrees. “If there’s one thing we’ve learned throughout the pandemic, it’s that you need a level of filtration to protect yourself against microorganisms,” he says. Medicom, a leading manufacturer and distributor of single-use and preventive infection control products for the medical, dental, government and industrial markets, constantly refines its products to be more effective against virus transmission. “In general, better filter media are thicker, but the tradeoff is always breathability.”
If you’re pining for a mask that provides extreme protection with no breathing resistance, that’s a long way off. Richard Cohen, Benco Dental’s managing director, is our go-to guy when it comes to PPE; he has spent more time than anyone we know visiting factories worldwide and delving deep into R&D. “You can’t have ‘easy breathing’ and ‘tight filter’ in the same product,” he says. Gary Steinberg, president of Medicom North America, agrees. “If there’s one thing we’ve learned throughout the pandemic, it’s that you need a level of filtration to protect yourself against microorganisms,” he says. Medicom, a leading manufacturer and distributor of single-use and preventive infection control products for the medical, dental, government and industrial markets, constantly refines its products to be more effective against virus transmission. “In general, better filter media are thicker, but the tradeoff is always breathability.”
That’s not to say manufacturers aren’t making improvements every year. Medicom markets a mask called SafeMask FreeFlow that uses “omega pleats” rather than shingle pleats: Two pleats face down, two up, creating an air pocket between the mask and the wearer’s face that, Medicom claims, allows air to flow more freely without affecting the level of protection. It was more than 35 years ago that 3M scientists started using an electrostatic charge to attract more particles to filter fibers. The result, 3M Advanced Electrostatic Media, has shown extremely low breathing resistance. “We can use less filter media and make it easier to breathe because you don’t need so much filter media in the respirator,” Dr. John Sebastian, a 3M respiratory research specialist, has said.
WHY NOT A LASER THAT CAN REPLACE BURS?
 Light has limitations. Burs have a more precise edge than lasers for the moment. Like all things, this will change with time—but how much time? We had zero luck nailing down any single expert for a prediction of when lasers might fully replace burs. Convergent Dental, maker of the highly regarded Solea laser, acknowledges that users will complete most preps with their laser and then refine using a traditional handpiece and bur, albeit with no need for anesthesia. What might spur that change?
Light has limitations. Burs have a more precise edge than lasers for the moment. Like all things, this will change with time—but how much time? We had zero luck nailing down any single expert for a prediction of when lasers might fully replace burs. Convergent Dental, maker of the highly regarded Solea laser, acknowledges that users will complete most preps with their laser and then refine using a traditional handpiece and bur, albeit with no need for anesthesia. What might spur that change?
Solea’s powerful light beam is optimized by a system called “galvos”: a series of microprocessor-controlled mirrors that move rapidly inside the laser’s arm. They’re capable of manipulating the beam thousands of times per second to create patterns expressly designed for the tissue being treated, whether enamel, bone, dentin or soft tissue. Energy is distributed in patterns whose diameters vary, enabling doctors to choose the perfect size for the job at hand. Galvos facilitates speed, precision and control unprecedented in a dental laser, Convergent says. Perhaps advances in laser and galvos technology will add even more precision, eventually spelling doom for drills.
WHY NOT SOMETHING BETTER THAN FLOSS?
 Floss as we know it was invented in the early 1800s by Levi Spear Parmly. The New Orleans dentist established the modern standard for flossing in his 1819 book, A Practical Guide to the Management of Teeth, which recommended that a waxen silk thread be run “through the interstices of the teeth . . . to dislodge that irritating matter which no brush can remove and which is the real source of disease.” So why do we still need the stuff? And why, after more than 200 years of innovation and technological evolution, hasn’t floss changed much?
Floss as we know it was invented in the early 1800s by Levi Spear Parmly. The New Orleans dentist established the modern standard for flossing in his 1819 book, A Practical Guide to the Management of Teeth, which recommended that a waxen silk thread be run “through the interstices of the teeth . . . to dislodge that irritating matter which no brush can remove and which is the real source of disease.” So why do we still need the stuff? And why, after more than 200 years of innovation and technological evolution, hasn’t floss changed much?
According to Dr. Jennifer Eisenhuth, founder of Dr. Jen Natural, a maker of nontoxic, cruelty-free, natural-ingredient dental products—including a plastic-free floss—flossing is still a necessary daily task for proper oral hygiene. “Flossing takes time and requires extra work, but the benefits last a lifetime,” she says. Plaque removal is something that neither brushing nor rinsing can accomplish. “Floss is the tool that disrupts the bond between plaque and teeth.”
So, OK, we can’t replace floss—but maybe we can make it better in the meantime. Though environmentally friendly floss isn’t exactly mainstream, those concerned with both oral health and microplastics can look at plastic-free products like Dr. Jen Natural’s as alternatives. “Microparticles break down in our mouths during flossing,” Dr. Eisenhuth says. “To avoid swallowing microplastics when flossing, switch to a natural silk floss. Silk is healthier for you and our planet.”
SURVEY
OPTIMISM IN THE WORLD OF IDEAS
What are your fellow dental professionals thinking about innovation these days? Here’s how Benco Dental customers responded to four probing questions.
What best describes your attitude toward the products and technologies currently available to doctors like you?
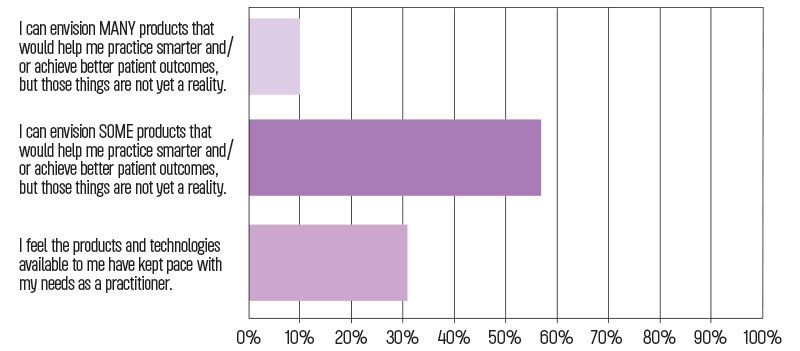
Dental R&D professionals, product planners and manufacturers have good reason to be proud of their work, according to the results of our survey. Fewer than 11 percent of respondents say they can envision “many” products that would help them practice smarter or achieve better patient outcomes, but that are not yet a reality. The majority—around 58 percent—say they can envision only some products that would help, and 31 percent agree that available products and technologies are keeping pace with their clinical needs. Overall, the results seem to
indicate very low dissatisfaction, with a healthy expectation for continual improvement.
In your experience, what factors, if any, most often prevent the development and sale of innovative or problem-solving products?
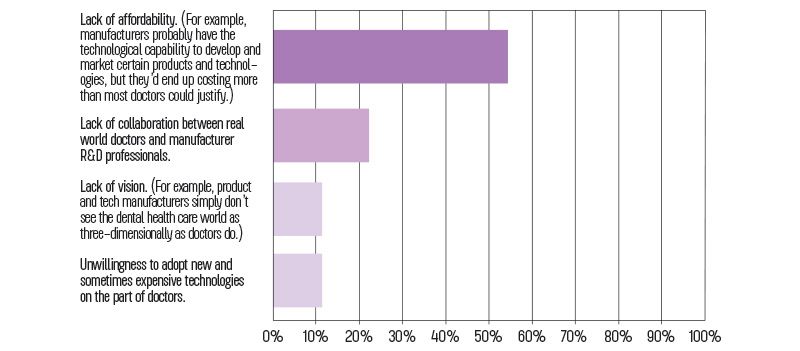
Here’s where the results get more interesting. About 54 percent of respondents say they believe manufacturers are able to produce more innovative products, but they would end up costing more than most doctors could justify. That represents another substantial vote of confidence in the ability of manufacturers to bring amazing products to market, if not necessarily inexpensively in the early adopter phase. About 22 percent cite a lack of collaboration between real-world doctors and R&D professionals as a bottleneck in the innovation pipeline, which perhaps indicates that manufacturers could do better at having two-way conversations with a larger population of end users. A small number of participants—slightly less than 12 percent—say tech manufacturers don’t see things as three-dimensionally as doctors do. Another nearly 12 percent cite unwillingness among doctors to adopt new and sometimes expensive technologies: a real bottleneck if ever there was one.
How often do you have ideas for new products and technologies that are not currently available but would help you practice smarter and/or achieve better patient outcomes?
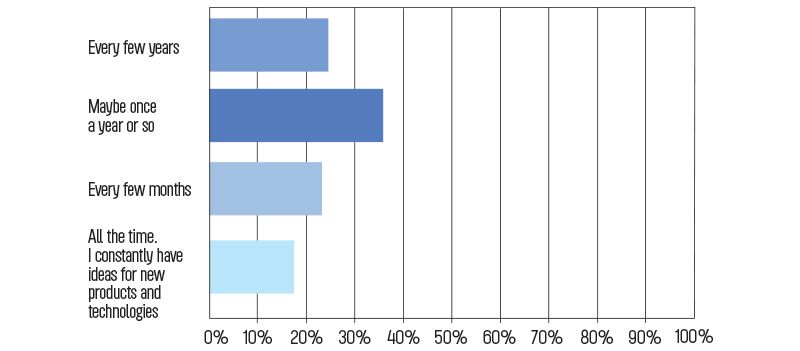
Doctors themselves report having a lot of ideas for new technologies: about 61 percent say they have new ideas maybe once a year or every few years, approximately 22 percent say they have ideas every few months and around 16 percent say they constantly have new ideas for products that would help them work smarter and deliver more effective care. Though there’s no direct correlation between this and the previous question about factors preventing the release of innovative products, it does seem to offer additional possible evidence that doctors have a lot more to say to manufacturers who are willing to listen.
Have you ever attempted to develop one of your ideas into a commercially viable product?
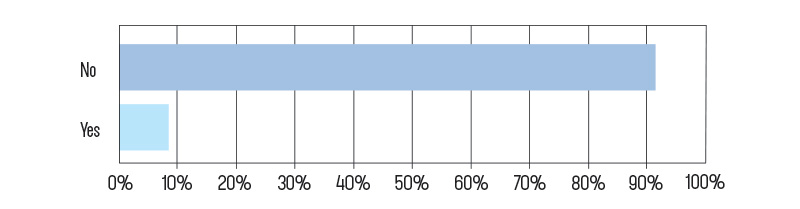
Finally, we asked our respondents if they’ve ever attempted to develop one of their ideas commercially. A little less than 9 percent say yes—which we feel is substantial. If you think of your friends in other professions, how many do you know personally who have taken a stab at inventing something?
OVERALL TAKEAWAYS:
The biggest seems to be confidence that manufacturers are capable of developing innovative products, if not necessarily at a widely accessible initial cost—a problem hardly unique to dentistry. But another takeaway is that doctors say they’re an idea-rich resource, at least some of whom will create products they want on their own if no one else will. While our survey was fairly informal, with a mathematical margin of error around 11 percent, we believe the results are more useful than that figure would suggest. (Unlike random surveys, ours was sent only to verified active customer accounts.) As a result, we’re excited by the general feeling of optimism, engagement and trust expressed by respondents.
WHY NOT ONE UNIVERSAL MATERIAL THAT ETCHES, PRIMES, BONDS AND RESTORES, ALL IN ONE?
Bill Grondin, senior manager, GC America, says the challenge is conflicting pH levels in the mouth (7.1, neutral, in a healthy mouth), tooth structure (about 5.5 for enamel) and the materials needed to restore the tooth. To prepare dentin or enamel to bond with a restorative, a phosphoric acid etch must have an extremely acidic pH of 0.1 to 0.4, but a final composite material needs a pH closer to the neutral pH of the mouth, with glass ionomers coming in at 3.9 to 4.7 and composites at about 6.0. The ideal solution would be to design one material that can morph in the oral cavity from highly acidic (like an etch) to neutral (like a restorative). So far, the closest we’ve come is a “one-step” composite or glass ionomer restorative. In the presence of lots of moisture, or when strength isn’t the primary consideration, a glass ionomer will work well and won’t require etching, rinsing or drying. When strength is more important, a composite is probably the right choice.
WHY NOT AN INTRAORAL SCANNER THAT’S AS SMALL AND AFFORDABLE AS AN INTRAORAL CAMERA?
The cost of high-quality intraoral cameras has plummeted from tens of thousands of dollars to under $350 in recent years, so why is an intraoral scanner still around $27,000 (the average of Benco Dental’s five most popular models)? We asked Patrick Strohkirch, director of sales at MEDIT, the global provider of 3D dental scanners and solutions.
“Intraoral scanners and cameras have different technologies,” he says. “Cameras are relatively simple in design, and their small size and affordability are due to the availability of compact camera technology. In contrast, scanners are used to create digital models of teeth and surrounding oral structures for various applications, such as restorative dentistry, orthodontics and implantology. Intraoral scanners use advanced scanning technology to capture detailed 3D images of the oral structures, and they require more complex hardware and software to operate.”
The good news: Scanner technology is advancing rapidly, with smaller, faster, more affordable models hitting the market. “Technological advances and market competition may eventually help make intraoral scanning technology more accessible to price-conscious dental professionals.”
WHY NOT A TOPICAL ANESTHETIC THAT TASTES BETTER?
 James Mulvahill has more than 15 years of FDA and pharma industry experience, centered prominently on anesthetics. Currently the chief operating officer of Wisconsin-based Bennett Pharmaceuticals of America, he tells us there are two considerations: First, most topical oral anesthetics are 20 percent benzocaine, and flavoring agents have a hard time overcoming its inherent taste. Second, why bother worrying how benzocaine-based topicals taste when the bigger issue, according to the FDA, is that benzocaine products “provide little to no benefit for the treatment of oral pain”? To that point, Mulvahill cites the FDA’s post-market drug safety information for patients and providers, “Safety Information on Benzocaine-Containing Products” (from 2018), as well as its “more recent podcast on drug safety, from January 20, 2022.”
James Mulvahill has more than 15 years of FDA and pharma industry experience, centered prominently on anesthetics. Currently the chief operating officer of Wisconsin-based Bennett Pharmaceuticals of America, he tells us there are two considerations: First, most topical oral anesthetics are 20 percent benzocaine, and flavoring agents have a hard time overcoming its inherent taste. Second, why bother worrying how benzocaine-based topicals taste when the bigger issue, according to the FDA, is that benzocaine products “provide little to no benefit for the treatment of oral pain”? To that point, Mulvahill cites the FDA’s post-market drug safety information for patients and providers, “Safety Information on Benzocaine-Containing Products” (from 2018), as well as its “more recent podcast on drug safety, from January 20, 2022.”
His own answer is Orlicaine Gel, Bennett’s patented topical made of tetracaine HCl, bupivacaine HCl and phenylephrine HCl. It has an appealing peppermint flavor, he says—and more importantly, Orlicaine’s active ingredients have been developed specifically for mucosal tissue. According to Dr. Mike Smilanich, a practicing dentist for more than 40 years and Bennett’s chief medical officer, it can be used for “anything that traumatizes or causes pain to the attached mucosa”—tissue management, frenectomies, biopsies—and “many extractions can be managed with Orlicaine alone.” The product was beginning to ship as of press time, so we’ll be watching to see how it’s received—but a member of the Incisal Edge team saw it in action at a recent Mission of Mercy event and came away impressed.