THERE WERE REALLY ONLY TWO TYPES OF ACCOMPLISHMENTS LAST YEAR:
The things we did because of the pandemic, and those we did in spite of it. For anyone working in any facet of dentistry, it was often a little bit of both. While 2020 may have slowed progress in some sectors, as you’ll see in the following pages, dentistry wasn’t one of them. Despite all the extraordinary challenges—including, lest we forget, an unprecedented wholesale industry shutdown—dentistry shone as a remarkable example of resilience, adaptation and, most of all, innovation.
For our first-ever issue of Incisal Edge devoted to the prior year’s innovation, we’ll introduce some exceptional people who pivoted smartly, stepped up cleverly or otherwise put their brainpower to work helping dentistry do its thing despite the virus. We’ll also look at noteworthy tech, products and trends that sent ripples through the industry. And we’d be remiss if we didn’t take a moment to celebrate everyday heroes like you who overcame, well, everything to continue delivering care amid crisis. With that in mind, it seems only fitting to kick off our look back at The Year in Innovation with two vital people who played a hugely important role in dentistry’s comeback.
OUR SINCEREST GRATITUDE to Dr. Rebecca Cornille, Dr. Setareh Lavasani, Dr. Carolyn Primus, Dr. Sheila Riggs, Dr. Kianor Shah and Dr. Paul Zhivago for their participation in Incisal Edge’s innovation panel discussion during this issue’s planning stages. Incisal Edge magazine
is solely responsible for all resulting editorial decisions.
MEN WITH A PLAN
The early days of the pandemic were a whirl of fear and confusion. Seeking to help dentists nationwide find their footing amid cataclysm, the ADA tapped
Drs. Rudolph Liddell (above left) and Kirk Norbo to head a task force of unprecedented urgency and significance. The leading players discuss how it all came together
to restore equilibrium to an industry in crisis.
By Elizabeth Dilts
LAST MARCH, WHEN governors nationwide ordered dental offices to close to all but emergency cases as states worked to keep residents at home and to preserve the limited supply of personal protective gear, the industry faced an emergency with no precedent.
The forced closure presented an existential threat to the businesses of many young dentists just getting their footing in their communities. Established dentists feared losing staff members permanently, as furloughed employees found other jobs and others were too afraid of contracting the virus to want to return to work.
A survey of more than 17,000 dentists conducted by the American Dental Association the first week of April found that 97 percent of dental offices were closed entirely or seeing only emergency patients, and around half had stopped paying their employees. Twenty percent said they were concerned their businesses would not survive until June if restrictions remained in place.
The ADA Board of Trustees endorsed the U.S. Centers for Disease Control and Prevention’s recommendation that dentists keep offices closed except to treat patients with urgent and emergency needs through the end of April. (They first voted for this step on March 16.) But ADA president Chad P. Gehani, a New York–based endodontist, knew that the group he headed needed to think hard about, and plan for, whatever lay ahead.
Trouble is, no one knew what that might be.
Dr. Gehani had a unique view into the threat Covid-19 presented, practicing just a few blocks from Elmhurst Hospital in Queens, New York, one of the epicenters of Gotham’s early battle against the epidemic. He anticipated that some areas of the country would reopen before others, and dentists would need guidance on how to treat patients safely. So in early April, he announced the formation of the Advisory Task Force on Dental Practice Recovery.
Doctors Rudolph Liddell and Kirk Norbo were named co-chairs of the committee, which included practicing dentists, infectious-disease experts and others. Their task was to create
a playbook where none existed.
“We had members asking us a cascade of questions, and we felt like if we didn’t have answers, we were letting them down,” Dr. Norbo says from his practice in Purcellville, Virginia. “If we didn’t do something, they’d be trying to navigate this and [figure out] how to protect their patients.”
Together, Dr. Norbo and Dr. Liddell had more than 70 years of dentistry under their lab coats; both had entered the profession during the AIDS crisis of the 1980s.
It was as a result of that pandemic that organized dentistry had been compelled to implement some of the strictest infection-control protocols in health care, raising its sanitation standards to the same level as those of any emergency room.
Three decades later, a better-armed ADA believed dentists could treat patients safely and prevent the spread of Covid-19 using mostly existing protocols—if they knew the mode of viral transmission.
In early April, though, the means by which Covid-19 spread were still unclear. It appeared to be passed through airborne aerosols, but guarding against those required personal protective equipment, which was nearly impossible to get.
I FELT EMPOWERED. I FELT LIKE I WAS MAKING A DIFFERENCE. I WOULD NOT WANT TO BE IN ANY OTHER POSITION THAN ON THIS TASK FORCE.
-DR. RUDOLPH LIDDELL
National PPE stockpiles were being doled out by the Federal Emergency Management Agency to health-care workers in order of its priority, and dentists were dismally low on the list. So as the ADA’s chief lobbyist, Michael Graham, worked to get dentists moved up, Dr. Liddell and Dr. Norbo got to work creating an industry tool kit.
On April 7, their task force held its first meeting, over Zoom. That night, Dr. Liddell says he lay awake thinking, “We have to come up with ideas every time we meet because we don’t know when we’re going to be given the green light to start practicing, and we don’t want to be late with our recommendations.
“The responsibility hit us after the first meeting,” he adds. “If we got this wrong, it could be devastating.”
Planning: A Need for Speed
Dr. Liddell had little time, though. He had been appointed by Florida governor Rick DeSantis to serve on the state’s committee on reopening. He had just finished, in 2019, his term as president of the Florida Dental Association, he was an ADA trustee and he still had his own two South Florida dental offices to manage.
Dr. Liddell says his peers would give him a virtual pat on the shoulder and say they did not envy him. His response: “I am not wringing my hands saying, ‘Boy, I hope we can figure something out, because what I’ve worked for my whole life is on the line.’ I felt empowered. I would not want to be in any other position than on this task force.”
Dr. Norbo had been tapped personally by Dr. Gehani for his background as an ADA trustee, a past president of the Virginia Dental Association and member of the ADA Council on Ethics, Bylaws and Judicial Affairs. He knew the group’s bureaucracy needed to do something it rarely did: work quickly.
“Timing was of the essence,” he says. “We were under the gun to perform in a short time. The ADA is sometimes likened to an aircraft carrier”—it can be slow and difficult to pilot in a different direction. “But this thing moved at warp speed.”
Starting April 8, the task force met three times weekly, for two hours each. Their discussions relied heavily on information provided by ADA researchers, who had been building
a dossier on the virus for weeks.
Working with Dr. Norbo and Dr. Liddell were Dr. Duc Ho, vice chair of the ADA’s Council on Dental Practice; Dr. Sarah Tevis Poteet, chair of the organization’s Council on Communications; Dr. Tom Paumier, a member of the Board of Trustees’ Budget and Finance Committee; Dr. Cody Graves, secretary-treasurer of the Texas Dental Association; and Drew Eason, executive director of the Florida Dental Association.
The task force discussed questions ranging from whether dentists should ask people to wait in their cars instead of the practice’s reception area to if offices needed to purchase state-of-the-art extraoral suction units.
Many answers were unknowable at the time. But the group created a Trello board—an online software workflow that each member could access—to organize their thoughts and research, and consulted with Marcelo Araujo, the ADA’s chief science officer and head of its Science & Research Institute.
They also called on contacts at the CDC and the Occupational Safety and Health Administration. They even called the American Society of Heating, Refrigerating and Air-Conditioning Engineers seeking input about air quality. “The information was disjointed at first, but it became more uniform,” Dr. Norbo says.
Every call ended with people running down their assignments for the next meeting. On April 27, the group presented its playbook for practicing in a pandemic to the ADA’s board of trustees.
Implementation: The Tool KIT
The Return to Work Interim Guidance Tool Kit, as it was called, provided practical resources for the weeks after reopening. It included a sample “welcome back” letter for patients, guidance for patient screening and in-office registration procedures, suggestions for how to prepare one’s reception area and protect team members, links to guidance on masks and a supplies shopping list.
In May, the task force added a hazard assessment guide and checklist that followed OSHA’s recommendations. In July, it added a flowchart to follow if a staff member or someone close to a staff member tested positive for Covid-19.
TIMING WAS OF THE ESSENCE. WE FELT LIKE WE WERE UNDER THE GUN TO PERFORM IN A SHORT PERIOD OF TIME.
– DR. KIRK NORBO
Around the same time, Graham, the ADA’s chief lobbyist, succeeded in getting dentists relabeled as essential workers by the federal government.
By January 4, 2021, the ADA had distributed 3.7 million N95 and KN95 masks and 786,000 gowns to roughly 62,000 dentists across the country. (Each dentist received at least one of these items.) The ADA reported that between April 27 and September 1, 2020, the kit’s website was visited 672,000 times and the primary document was downloaded 36,000 times. Dr. Liddell’s feeling of empowerment had trumped his colleagues’ assumption that the task force might end up a snarled, bureaucratic mess. As a result, the dental industry overall has made it through the pandemic—and continues to do so—in admirable shape, able to return to providing care to patients who are, fitfully, returning to the chair.
“We didn’t get a ribbon for being first,” Dr. Liddell says. “But because the group realized the enormity and significance of what we were doing, everyone was so focused that we
got it out in time.”
PEOPLE OF 3M
 The PPE Production Multipliers
The PPE Production Multipliers
No kind of conventional planning or forecasting could have prepared 3M for the pandemic. Yet the company managed to triple its 2019 respirator production last year, to more than 2 billion units globally.
Though sheer determination certainly played a part, it seems the accomplishment is more a byproduct of 3M’s forward-thinking culture and dedication to agility. The former is the yield of brutally taxing work such as running production lines nonstop, adding new lines and refitting old ones for respirator production. The latter seemingly has to do with lessons 3M learned from SARS, plus leveraging advanced supply-chain technology not only to manage shipping but also a complex multinational web of suppliers. It has been a staggering logistical feat that simply can’t be attributed to any single person (though we have previously acknowledged Eric Wenzel, the company’s director of oral care global business, as No. 1 on our 2020 list of the 32 Most Influential People in Dentistry).

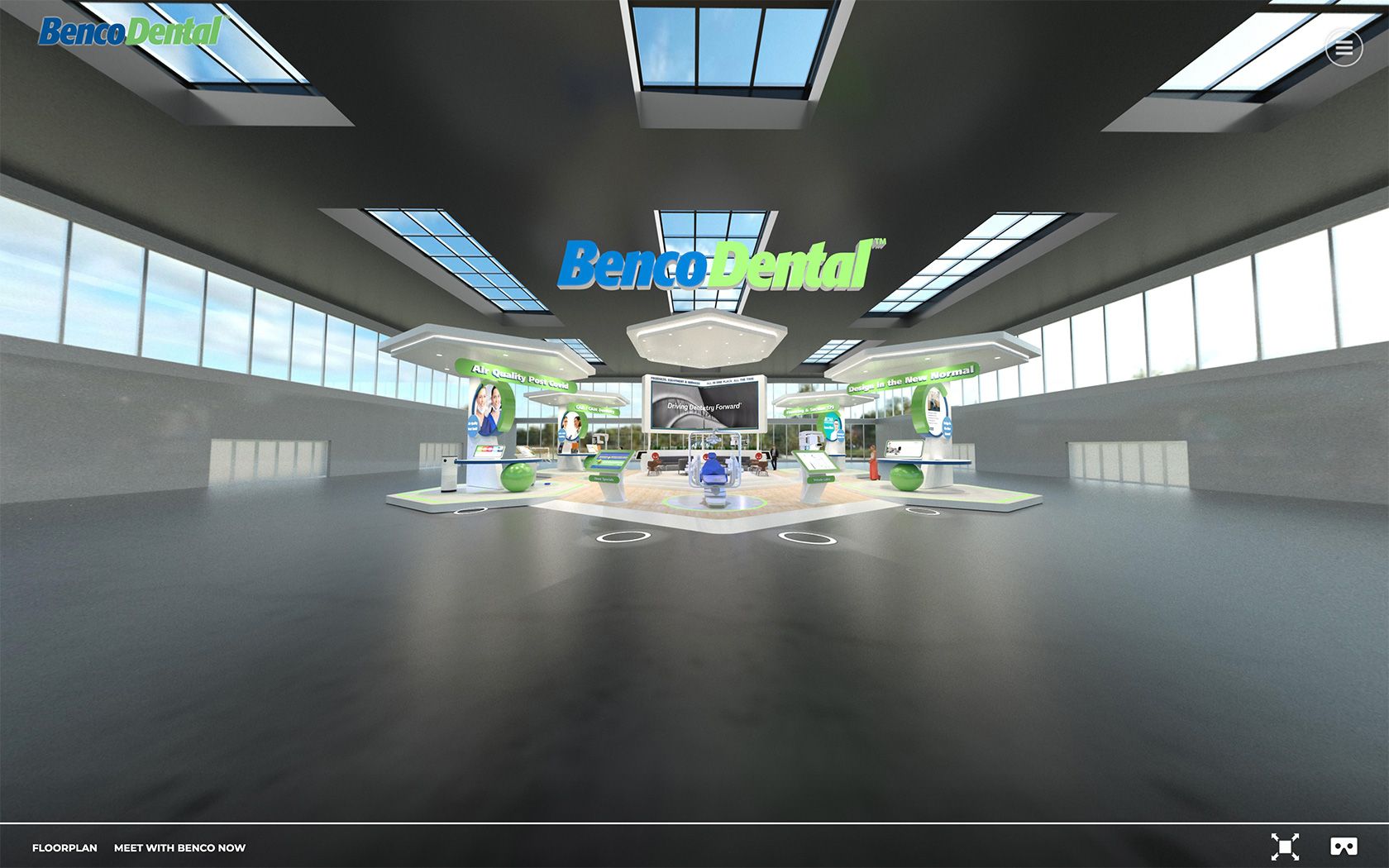
VIRTUALLY FAMILIAR
As dental meetings moved online, Benco Dental’s events team worked with software engineers to create a comfortingly recognizable trade-show booth for the company. “Taking an immersive approach allows people to experience it in the same way they’d walk through a real exhibit, but with the addition of enhanced VR features,” says Benco’s Lindsay Pross. “Approximating something approaching normal through technology is hopefully both soothing and engaging.”
A PANDEMIC BRIGHT SPOT
CONVERGENT DENTAL
SOLEA LASER
 The pandemic forced dentistry to consider lasers in, ahem, a new light. After all, capturing aerosol is perhaps not as critical if there’s less of it in the first place. Plus, faster procedures are great for boosting productivity levels. We caught up with New York’s Dr. Jaime Bremnes, a Solea user we spoke with near the start of the Covid crisis, for an update. “Patients are leery about spending time without their masks on,” she says. “Solea gets patients in and out very quickly.” All that, plus less fluids and no need to wait for anesthesia, mean Solea gets a place on our shortlist of innovations that became even more relevant during 2020.
The pandemic forced dentistry to consider lasers in, ahem, a new light. After all, capturing aerosol is perhaps not as critical if there’s less of it in the first place. Plus, faster procedures are great for boosting productivity levels. We caught up with New York’s Dr. Jaime Bremnes, a Solea user we spoke with near the start of the Covid crisis, for an update. “Patients are leery about spending time without their masks on,” she says. “Solea gets patients in and out very quickly.” All that, plus less fluids and no need to wait for anesthesia, mean Solea gets a place on our shortlist of innovations that became even more relevant during 2020.
Unlike some major equipment investments, Solea offers a new way to help pay for itself, too. More than 60 percent of adults snore. Solea Sleep, launched mid-2020, is a single-treatment solution that takes less time than whitening. It painlessly tightens the soft palate, reducing vibrations that cause snoring. “The tissue is gently warmed at the perfect depth in the soft palate, resulting in instant results,” wrote Dr. Yooson Kim in a recent article. With an average cost to treat of $1,000, and 90 million people who snore, it makes the prospect of laser dentistry even more exciting.
DR. DANIEL GERMAN
THE MIND BEHIND EXPANDING ORTHO ACCESS
Founded in 2016, Orthobrain delivered a new approach for general dentists to offer comprehensive ortho treatment beyond mere aligners. Dr. Daniel German, a former large-practice orthodontist, pioneered the subscription model for orthodontic support at a time when it was just gaining steam in consumer products as varied as razors (Dollar Shave Club) and automobiles (Care by Volvo).
A true breakthrough moment may have come for Dr. German in 2020, though: The pandemic suddenly shifted patient preferences toward fewer visits and providers, while general dentists struggled to find new revenue sources to claw back from the financial hardship of the shutdown.
Last year, Orthobrain more than tripled its number of registered dentists over 2019. And an entire patient population who otherwise wouldn’t seek out an orthodontist—and would therefore go untreated—is benefiting. “We have successfully transformed the way orthodontics can be delivered,” Dr. German says, “allowing general dentists to deliver excellent care with the expertise of specialists providing the planning, support and education.”
WE HAVE SUCCESSFULLY TRANSFORMED THE WAY ORTHODONTICS CAN BE DELIVERED.
– DR. DANIEL GERMAN
EXPONENTIAL IMPROVEMENT
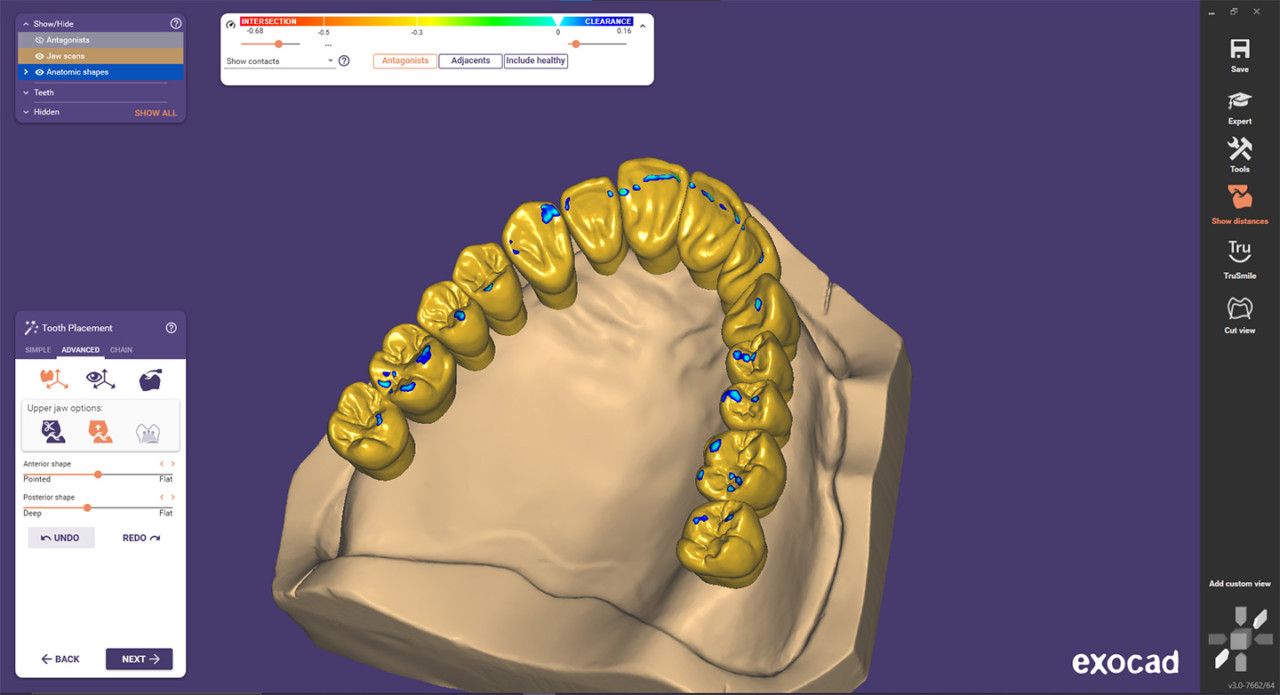 exocad DENTALCAD 3.0 GALWAY SOFTWARE
exocad DENTALCAD 3.0 GALWAY SOFTWARE
The exocad development team continues to push its software solutions closer to melding smartphone-app-like simplicity with powerful functionality. Dropped late last year, DentalCAD 3.0 Galway revolutionizes the design process for the occlusal aspect of dental restorations with a new Instant Anatomic Morphing tool. It eliminates the individual positioning movements, rotational corrections and fine adjustments to the surface that are required using different tools and functions when modifying the placement or anatomy of a proposed design.
Now, all changes can simply be applied simultaneously. Plus, the entire arch can be manipulated by a single slide that defines the depth of the occlusion. Even more exciting, exocad hints at the advances to come when exoplan 3.0 Galway for guided surgery becomes available following 510(k) clearance from the FDA. Until then, DentalCAD 3.0 Galway saves major time—and headaches—for dental labs, prosthodontists and general practitioners faced with complex treatment planning and restorative designs.
Dr. BRYAN LASKIN
TELEDENTISTRY’S SYMPHONY CONDUCTOR
 Minnesota independent dentist and tech entrepreneur Dr. Bryan Laskin might not have seen the pandemic coming, but his company was already positioned to respond. OperaDDS has been at the forefront of digital patient communications, providing an integrated platform that tames the jumble of patient forms and screening tools to make it all manageable—a boon for IDPs who don’t have the time, experience or budget for custom tech solutions.
Minnesota independent dentist and tech entrepreneur Dr. Bryan Laskin might not have seen the pandemic coming, but his company was already positioned to respond. OperaDDS has been at the forefront of digital patient communications, providing an integrated platform that tames the jumble of patient forms and screening tools to make it all manageable—a boon for IDPs who don’t have the time, experience or budget for custom tech solutions.
Dr. Laskin’s team also had a comprehensive Covid-19 patient-screening and teledentistry product ready during the early stages of the pandemic. “The way doctors and patients communicate is changing fast by necessity, and more people will be sharing information electronically than ever before,” Dr. Laskin says. “Our solutions ensure they can do so confidently, and also easily, since many patients with limited technology exposure will need to adapt.”
MAKING PHILANTHROPHY SUSTAINABLE

A nonprofit that depends less on donations is a healthier nonprofit. Twice, the cleaner toothpaste brand founded by Julian Levine, Cody Levine and rocker Lenny Kravitz, is possibly the coolest on the market. Which is good for those in need, since profits help fund the GLO Good Foundation—the philanthropic arm of GLO Science, the company run by Julian and Cody’s parents, Manhattan dentist Dr. Jonathan B. Levine and his wife, Stacey.
—Incisal Edge, Spring 2020
THE PLUMMETING PRICE OF 3D IMAGING

 Fun fact: In 1978, a 25-inch console TV sold for $775 at Sears—adjusted for inflation, that’s about $3,200. In 2021, you can walk away from Best Buy with a 75-inch LED 4K for $775 in today’s money. While technology hasn’t really made a carton of milk or a loaf of bread any cheaper, it has certainly done so when it comes to cutting-edge electronics like high-def TVs . . . and high-def imaging.
Fun fact: In 1978, a 25-inch console TV sold for $775 at Sears—adjusted for inflation, that’s about $3,200. In 2021, you can walk away from Best Buy with a 75-inch LED 4K for $775 in today’s money. While technology hasn’t really made a carton of milk or a loaf of bread any cheaper, it has certainly done so when it comes to cutting-edge electronics like high-def TVs . . . and high-def imaging.
Dentistry has been a big beneficiary, as the price of 3D X-rays has been slashed in half during recent years. It wasn’t long ago that a 3D pan could easily cost upward of $100,000. Now it’s more like $50,000 to $60,000 for a medium-field-of-view unit with features and performance eclipsing that of a six-figure unit from not long ago. For a lot of doctors, that’s the difference between inaccessible and accessible. And for patient populations nationwide, it opens the door for new treatments from their providers.
Over the years, 3D has been one of this magazine’s most talked-about subjects. “Implants and airway management with 3D technology has been a game changer,” Dr. Nikki Jones Bailey told Incisal Edge. “I love my 3D X-ray technology, which enables a more comprehensive diagnosis and helps me plan accurate, minimally invasive implant surgeries.” Added 40 Under 40 alumnus Dr. Daniel Coleman: “With 3D anatomic information, we’re able to safely and effectively plan ideal treatment for our patients.” Another 40 Under 40 alum, Dr. Chad Matthews, echoed the sentiments of many, telling us of 3D cone beam technology: “Once you start using it, it’s very difficult not to use it.”
SCHOOL’S OUT
Zoom classes are hardly a panacea if the power gets cut: how the pandemic has battered dental education in the developing world.
By Dr. Yasir Israr
EDUCATORS WORLDWIDE, like everyone else, have had to radically alter the way they do business since the onset of the pandemic early last year. In many places, that meant a shift to Zoom classes and perhaps socially distanced class time—an irritant, perhaps, but ultimately smoothly executed and hardly fatal to the cause of learning.
Despite the large amount of theoretical knowledge inherent to the discipline, dental education still encompasses a great deal of practical procedures and community interaction. As such, educational institutions in the developing world—where infrastructure and funding for technology sorely lag the West—have struggled since the advent of Covid-19.
In many of these places, the very idea of remote electronic schooling was an alien concept, and institutions were unprepared for this sudden shift. (Some schools don’t even operate an official email system, lacking the necessary IT support to make it worthwhile.) As strange as it sounds to American ears, many teachers in the developing world use their phones and computers for little more than calls and messages. Getting them comfortable with instruction-by-video presented a substantial challenge.
Socioeconomics, of course, is an unavoidable factor. Many dental students come from poor families and are able to attend school solely through scholarships or loans; a new phone or computer can be a prohibitive expense. Moreover, an internet connection fast and reliable enough for a smooth, stable connection is still a luxury in many parts of the world. Students forced by the pandemic to return home to rural areas felt this even more acutely, with some forced to choose between the expense of renting an urban space with better connectivity or putting their education on hold.
Some teachers recorded their lectures and sent them to students to download and view later—a solution, if an imperfect one when faculty had to come to the school and get assistance from a third party to record and edit the material.
The ability to pull off anything other than a traditional lecture, meanwhile, was highly circumscribed. Creative pedagogy isn’t easy when you’re limited to screen sharing or simple PowerPoint presentations. Surveys indicated, no surprise, that student engagement plummeted, with some merely amusing themselves online while ostensibly logged into class.
Yet another hurdle: the fact that dental education relies heavily on practical tutorials, three-dimensional models and patient interaction. Dental schools in socioeconomically deprived nations have limited means to teach clinical skills, the bulk of which stem from direct patient observation, as well as supervised and assisted learning. Students wishing for more have had to scavenge tutorials of dubious utility off platforms like YouTube.
Online exams present further problems. Using multiple cameras or custom software to keep an eye on students isn’t tenable; many schools therefore improvised with timed questions and unorthodox material—methods hampered by the same old connection trouble and software glitches.
All these factors, tragically, have in some countries essentially forced a cessation of adequate dental instruction. Urgent financial assistance and streamlined procedures at both the governmental and local level can help, but there are no magic fixes—only dismay at the uncountable ways this terrible pandemic has added further burdens to developing countries’ already heaping load.
DR. YASIR ISRAR is a resident orthodontist at Gandhara University in Peshawar, Pakistan.
Dr. MIC FALKEL
THE PANDEMIC’S PERFECT PIVOTER
 For years, anesthetic buffering has been gaining traction among dentists who understand that a few minutes saved per patient adds up quickly—and also that more comfortable and profound anesthesia sets a practice apart. When the CDC issued Covid-19 guidelines urging dentists, when possible, to stay with patients throughout their entire procedure, anesthetic buffering became an essential tool for enhancing safety while conserving precious PPE.
For years, anesthetic buffering has been gaining traction among dentists who understand that a few minutes saved per patient adds up quickly—and also that more comfortable and profound anesthesia sets a practice apart. When the CDC issued Covid-19 guidelines urging dentists, when possible, to stay with patients throughout their entire procedure, anesthetic buffering became an essential tool for enhancing safety while conserving precious PPE.
Cue Dr. Mic Falkel’s labor of love: the Onset buffering system. Onset instantly raises the pH of local anesthetic at chairside, taking the patient’s physiology out of the buffering process and leading to a 6,000-fold increase in the amount of available active anesthetic. This makes for a comfortable anesthetic injection that works more quickly and predictably. “I knew as far back as dental school that you could build a practice around providing a more comfortable injection,” says Dr. Falkel, founder and chief medical officer of Onpharma. “But for years, I looked for ways to improve local anesthetic even more.” It seems he has, judging by the product’s growing cadre of new enthusiasts.
They’re joining some prominent longtime proponents like Dr. Stanley F. Malamed, who literally wrote the book on local anesthesia. “I sound like I’m a salesman for Onpharma, but I’m not,” Dr. Malamed says. ”I’ve even come to the point where I conclude all my lectures with it.”
CRUCIAL CONNECTEDNESS
DENTALEZ AERAS UTILITY AND HANDPIECES
You use software and apps to connect to everything: your lighting, your kitchen appliances. Yet those are hardly as important as your mechanical room, the beating heart of your practice. The new Aeras Intelligent Platform from DentalEZ aims to change that. It’s designed to “save energy, waste and reduce unplanned downtime while minimizing disruptions for an increased focus on patients,” according to the company’s president, Heather Trombley.
The new Aeras Compressor and Vacuum by Ramvac use cloud-based technology for monitoring via embedded sensors to detect potential problems so they can be addressed before trouble arises. Meanwhile, the 500 Elite Handpiece by Star employs RFID technology to help users track handpiece usage, monitor sterilization and view location data for added assurance without the hassles of traditional recordkeeping.
COOPERATION NATION
One pandemic silver lining: the rapid adoption of collaboration tools for both communication and treatment.
A PHRASE NO ONE used at the start of 2020 became a tiresome term as the pandemic wore on: social distancing. One problem for the industry in which we all ply our trade: Dentistry is pretty much the antithesis of social distancing. As with so much else last year, though, cue the technological innovation: To the extent dentistry can be practiced with distance in mind,
it’s being done.
“In some senses, collaboration between dental professionals has been even more efficient since the beginning of the pandemic because of the way we’ve utilized technological tools,” says Dr. Kianor Shah, a dentist and entrepreneur in Palm Desert, California. He points in particular to the ease of information sharing that virtual-networking tools have provided from the beginning of the coronavirus disruptions a year ago. “When the pandemic began, we had to figure out ways to keep our networks connected,” he continues. “We thought, why not take some of the best thought leaders in the industry and put them on a Zoom conference? That way we can have an even bigger audience than we could in a physical room.”
That’s not hyperbole: The virtual conference Dr. Shah helped organize spanned five continents, with dental experts from across the globe—and thousands of dental professionals in the audience—adding their input on how practitioners could mitigate the worst of the lockdowns and difficulties engendered by the vagaries of the pandemic. Social media, no surprise, was a major factor in getting so many disparate pros together.
That confab was only the beginning, however: “Thanks to virtual conferences and social media, we’ve been able to extend our reach to over 2 million dentists across the globe,” Dr. Shah adds. “These virtual conferencing tools can help eliminate some of the expenses that create barriers to networking. They’ve been very valuable.”
Of equal importance, however, is the way such virtual tools have helped dentists in their day-to-day practice. A doctor in full PPE mufti treating one patient can share information, medical files, scans and a thousand other things instantly with colleagues, labs, academics and others—a degree of collaborative care that was all but unknown even a decade ago, and one whose adoption was significantly accelerated, out of necessity, by Covid-19.
“Since everyone across the industry has had to adapt to using these virtual collaboration tools, it’s made them easier to use with a team,” says Dr. Paul Zhivago, a practitioner in Manhattan and a professor at New York University’s College of Dentistry. “With all the different specialties that can go into helping a patient, it’s important that we’re all on the same page. Each specialist might have a different approach to the same patient issue, so it’s especially great to be able to speak with experts in real time to figure out what the best care solutions are.” —Sean Devlin
PORTABLE PANO
 Cathy J. Grinham, one of Massachusetts’ first dental hygienists licensed to provide preventive care outside the dental office, needed an imaging solution for her nursing-home patients with dementia and mobility problems. She decided to invent her own. That’s how the wheelchair-friendly Portable Panoramic Imaging System was born—and why we honored her with an Innovation nod in our seventh annual Lucy Hobbs Awards.
Cathy J. Grinham, one of Massachusetts’ first dental hygienists licensed to provide preventive care outside the dental office, needed an imaging solution for her nursing-home patients with dementia and mobility problems. She decided to invent her own. That’s how the wheelchair-friendly Portable Panoramic Imaging System was born—and why we honored her with an Innovation nod in our seventh annual Lucy Hobbs Awards.
—Incisal Edge, Winter 2020
CLASS STRUGGLE
Reimagining dental education in a post-pandemic world.
 WHEN COVID-19 took hold in the U.S. last spring, teachers across the country had to adjust their methods, medical educators in particular. You can discuss Twelfth Night easily over Zoom, say, but how do you transfer a lab to the virtual realm?
WHEN COVID-19 took hold in the U.S. last spring, teachers across the country had to adjust their methods, medical educators in particular. You can discuss Twelfth Night easily over Zoom, say, but how do you transfer a lab to the virtual realm?
“Since the outbreak, we’ve managed to move our educational work online,” says Dr. Paul Zhivago, who teaches at New York University College of Dentistry, noting that he and his colleagues have been able to fully integrate at least some portions of the curriculum online.
Some schools were even further ahead of the curve. “Five years ago, we started to put all our content in a digital platform,” says Dr. Setareh Lavasani, an associate professor at Western University College of Dental Medicine in Pomona, California. “It’s been working amazingly well for our students, so our transition was easier.”
Dr. Zhivago echoes that. “In just two months, we were able to completely transfer our modules online for our students to use,” he says. “It was a really involved process to get everything integrated, and we’re proud that it’s worked out as well as it has. The software we use is complex and requires more time, so [students] being able to rewatch [lectures] isn’t a bad thing.”
Dr. Sheila Riggs, an associate professor and chair of the Department of Primary Dental Care at the University of Minnesota, extols the virtues of distance learning but is quick to add that optimal clinical work requires students to come back as soon as possible—something she says can be done in a limited way with smaller class sizes and more PPE than normal.
In all, Dr. Riggs is optimistic that the doctors of tomorrow will still thrive. “While students learning during the pandemic will still be competent practitioners, it’s true that they’ll have fewer hours in clinic,” she says. There’s a silver lining to that, though: “They’ll come to appreciate infection-control procedures in the future due to their current experiences.” —S.D.
DR. MERT N. AKSU, JD, MHSA
The Relentless Visionary
 Many dental-school deans and professors across America were heroes of the pandemic, but Dr. Mert N. Aksu capped off his year by being named a recipient of the prestigious American Dental Education Association’s Gies Award for Vision—Dental Educator. Throughout his career, and as dean of the University of Detroit Mercy’s School of Dentistry, Dr. Aksu has been a constant challenger of the status quo, leading what his colleagues characterize as an extraordinary response to Covid-19 that included co-inventing an FDA-approved, patent-pending aerosol mitigation system used with units in the dental clinic.
Many dental-school deans and professors across America were heroes of the pandemic, but Dr. Mert N. Aksu capped off his year by being named a recipient of the prestigious American Dental Education Association’s Gies Award for Vision—Dental Educator. Throughout his career, and as dean of the University of Detroit Mercy’s School of Dentistry, Dr. Aksu has been a constant challenger of the status quo, leading what his colleagues characterize as an extraordinary response to Covid-19 that included co-inventing an FDA-approved, patent-pending aerosol mitigation system used with units in the dental clinic.
His work also helped the clinic remain open to treat emergency patients during the school’s shutdown. Not surprising, since he led the planning of Mercy’s renovation in 2006 and, in 2019, worked with Dr. Melanie Mayberry to form a partnership with Oakland University’s William Beaumont School of Medicine to bring together second-year students to share case studies and collaborate for better outcomes. The Gies Award cements his reputation as a creative leader as well as a forward-looking, passionate and dedicated educator.
INTERDISCIPLINARY TEST
 Walmart Health is slowly adding dentistry to its clinics. And the company’s head of dentistry, Dr. Roshan Parikh, is a strong proponent of leveraging this opportunity to drive the adoption of integrated care. Though often talked about, the idea hasn’t seen much actual adoption. Could a retail juggernaut like Walmart be the ultimate catalyst for change? Stay tuned.
Walmart Health is slowly adding dentistry to its clinics. And the company’s head of dentistry, Dr. Roshan Parikh, is a strong proponent of leveraging this opportunity to drive the adoption of integrated care. Though often talked about, the idea hasn’t seen much actual adoption. Could a retail juggernaut like Walmart be the ultimate catalyst for change? Stay tuned.
—Incisal Edge, SUMMER 2020
MACHINE-LEARNING REVOLUTION
OVERJET AI, PEARL, VIDeAHEALTH
Artificial intelligence is here, and with it comes the prospect of faster, more accurate diagnoses and compelling case presentations. The mere idea of a supersmart digital assistant was the stuff of dreams not long ago. Yet it was only in the last couple years that viable products emerged—and not from where we necessarily expected.
This exciting world, at least so far, belongs to young startups rather than resource-rich dental conglomerates. Pearl and VideaHealth got major cash infusions in 2019, but 2020 saw Overjet AI raise $7.85 million in a seed round led by VC Crosslink Capital, and perhaps emerge as the potential industry leader. Incisal Edge named Overjet’s CEO, Dr. Wardah Inam, to our 2020 list of the 32 Most Influential People in Dentistry. According to Dr. Inam, AI “encodes dentists’ understanding of disease identification and progression into precise, bias-free and repeatable frameworks for better decision making.” Plus, the potential for AI to accelerate the pace of clinical research is yet another facet yet to be fully tapped. Keep an eye on all three companies—and on this rapidly expanding space. More entrants are surely on the way.
OPERATORIES ONLINE
Acceptance of teledentistry got a rocket-fueled boost during virus lockdowns. is it here to stay?
FEW PROFESSIONS are as ill-suited to social distancing as dentistry, as literal an in-your-face discipline as exists. Many medical specialists—and regulators—have long frowned on telemedicine, but that distaste is just one of the many longstanding conventions jettisoned last year.
Teledentistry isn’t entirely new, of course, no matter how bright its current moment. Dr. Rebecca Cornille, chief dental officer at the Vista Community Clinic in California, has been employing digital techniques with patients for some time now. “We’ve been using teledentistry for several years through a pilot program with the State of California,” she says. “The ‘Virtual Dental Home’ is a concept of asynchronous telehealth that we’ve used to go to patients, rather than requiring an office visit. When Covid-19 created access issues and barriers to care, we modified the process to complete synchronous telehealth. It has allowed us to assess patients over video and determine the need for an in-clinic visit. It’s incredibly advantageous—it can keep the patient at home when an in-person visit is not necessary, expedites an in-clinic visit if one is deemed necessary and allows for access and continuity of care for patients in need during a very challenging time.”
Heady stuff. It has also been a boon to patients who need urgent care, whether they know it or not. “In our teledentistry platform, Dentulu, the patient is matched with a licensed dentist in that state who can address the emergency and prescribe medicines if necessary,” says Dr. Arash Hakhamian, a dentist in Los Angeles and the cofounder and CEO of Dentulu.
Dentulu and platforms like it don’t merely streamline the process of providing care; they also help doctors reach patients in “dental deserts” where care options are scarce to nonexistent. “Our platform is making dental care accessible to all people across the United States,” Dr. Hakhamian says. “Many people in underserved communities or remote rural areas have little to no access to quality care. Dentulu bridges that gap by making care available online. This eliminates the cost and potential health risks of traveling to a clinic in person—particularly important during a pandemic.”
Increasing vaccination rates throughout 2021 will render teledentistry something less than an utter necessity—but the odds seem good it has sunk roots and is here to stay. —S.D.
SAY CHEESE
What’s the one thing people want most on social media? A share-worthy photo of themselves, of course. That’s why Dr. Marina Ambridge established a real-deal photo studio—complete with makeup artist—at her Arizona practice, the Smile Institute. Unsurprisingly, her delighted patients share away to show off their new smiles . . . and their friends on Instagram and Facebook often become Dr. Ambridge’s newest patients.
—Incisal Edge, FALL 2020
HOSPITAL FLOW
Hospitals have well-defined rules for how they’re designed; that’s why they’re typically so streamlined and efficient. Dental offices, however, don’t. So Benco Dental’s CenterPoint designers developed an industry-first hybrid of best practices in alignment with entities like the CDC, OSHA and WHO that contribute to approved guidelines required by the Department of Health for hospitals. The result: hospital-grade people flow for dental environments.
—BENCO DENTAL’S LEARNING CENTER
Aerosol Capture’s Emergence
 As practices reopened following dentistry’s shutdown—and after a wave of hysteria that included talk of mandating negative-pressure rooms—cooler heads prevailed, enhanced PPE became the norm and dentistry marched on. Yet the appetite for aerosol-capture devices grew steadily in 2020. Entering the dental market were new players including Nederman, which applied its 76 years of clean-air experience in industrial settings like factories to a much smaller scale.
As practices reopened following dentistry’s shutdown—and after a wave of hysteria that included talk of mandating negative-pressure rooms—cooler heads prevailed, enhanced PPE became the norm and dentistry marched on. Yet the appetite for aerosol-capture devices grew steadily in 2020. Entering the dental market were new players including Nederman, which applied its 76 years of clean-air experience in industrial settings like factories to a much smaller scale.
Nederman’s approach uses flexible arms that mount to the wall or ceiling and, ideally, push outdoors as exhaust what they capture. Other manufacturers—ADS, EnviroKlenz, Vaniman, Flight and more—offer a host of aerosol-capture options.
Then there are the products that found an enhanced sense of purpose amid the pandemic. Kulzer’s Ivory ReLeaf system, launched as a hands-free HVE suction device, found plenty of users who embraced it for aerosol reduction, if not capture. Its leaf-shaped mouthpiece offers about 280 degrees of suction, far more than a traditional saliva evacuator. The Zyris Isolite 3 dental isolation system is another well-regarded product that was originally designed to provide an extra set of hands but was embraced in 2020 as a way to reduce aerosols and their attendant risks. Combining those with ambient air-quality solutions, plus active PPE such as powered air-purifying respirators, delivers a multilayered approach to risk mitigation that will likely be
part of everyday dentistry from now on.
THE BIG ASK
THE YEAR OF COVID-19 LEFT DENTISTRY WITH A HOST OF UNANSWERED QUESTIONS GOING FORWARD.
FEW YEARS IN living memory began with so many uncertainties as did 2021. Professionals of all stripes have had to figure out how to operate, how to move forward and, in many sad cases, how just to keep the lights on and stay in business. Dentistry as an industry has shown remarkable resilience after nearly a year of disruption, but a number of things remain uncertain as the world begins its slow emergence from Covid-19.
What role will midlevel providers play? Few maintain a studied neutrality when it comes to this controversial group, but in an era when expanding access to oral care is a top priority, midlevel providers surely have a role to play. Dr. Sheila Riggs, an associate professor and chair of the Department of Primary Dental Care at the University of Minnesota, says that maintaining a cooperative, team-oriented approach going forward will be the best solution for patients and providers alike. “At the University of Minnesota, we’ve been educating all three members of the oral health team: dentist, hygienist, therapist,” says Dr. Riggs, whose state has long been preeminent in permitting and educating midlevel providers. “The therapist focuses on prevention. We’ve got to have a collaborative approach to reach people in underserved communities. Thus far, we’ve been pretty successful in Minnesota in making sure these midlevel providers are looked after. When the team is able to work in harmony, it’s the best outcome for all parties involved.”
What about disenfranchised patients? It has long been a truism that when people lose their jobs and their health insurance, dental care is often the first to fall by the wayside. This is in large part a public-policy question for lawmakers, of course, but longtime proselytizers for teledentistry—Dentulu founder and CEO Dr. Arash Hakhamian is one such apostle—see endless possibility for dentistry-via-app that removes some of the high hurdles currently blocking patients whose hold on their dental care is tenuous.
Dr. Carolyn Primus, recipient of the Innovator Award as part of the 2020 Lucy Hobbs Project, knows that minimally invasive dentistry means less of it—a potentially key factor for patients with limited time, money and insurance. “What I’ve focused on this year, as every year, is preservation of dentition,” Dr. Primus says. “We always have to think about minimally invasive dentistry. It’s good for both our current era, with the pandemic, and it’s good long-term for the patient.”
Regardless of when dentistry will return to “normal,” many think the industry is on the right track, pocketing lessons learned during the pandemic to streamline operations and care delivery in the near term. “The dental industry will experience massive growth and consolidation over the next five years, with corporate interests investing billions of dollars,” says Dr. Hakhamian. “Dentists will have to catch up with technology advances such as teledentistry, robotics and mobile dentistry. These will not only increase access to care, but they’ll also create innovative ways for
new dentists to generate revenue. It’s the future of our field. This will be advantageous to doctor and patient alike.” —S.D.
3D PRINTING: INNOVATION TAKING SHAPE
SHARON SOONG, MATERIALS LEAD FORMLABS
 Between creating industrial materials for Google and pitching in during the race to accelerate ventilator production, Formlabs—based in Somerville, Massachusetts, just outside Boston—further expanded its influence as a leader in the 3D-printing space throughout 2020. Incisal Edge spoke to Sharon Soong about where the industry is headed, and what upcoming advances will mean for dentistry.
Between creating industrial materials for Google and pitching in during the race to accelerate ventilator production, Formlabs—based in Somerville, Massachusetts, just outside Boston—further expanded its influence as a leader in the 3D-printing space throughout 2020. Incisal Edge spoke to Sharon Soong about where the industry is headed, and what upcoming advances will mean for dentistry.
Where will the biggest advances likely be happening: in printers or materials?
Advancements in material science are key to the growth of 3D printing in industries like dentistry. Having materials that provide a new level of utility and simplify workflow for users is key to highlighting the value 3D printing provides to both their offices and their patients. It opens a new pathway for dental offices and labs to deliver quality products with low upfront cost for long-term restorations, molds, prosthetics and more.
What are the practical applications for all these new materials?
Formlabs has a library of more than 20 resins for the dental industry. As part of our Materials Partnership Platform with BEGO, a leading specialist in the field of prosthodontics and implant dentistry, we introduced new resins that enable 3D printing of dental restorations like crowns, bridges, inlays, onlays and veneers for the first time. The Permanent Crown Resin, for example, features high strength and low water absorption required for long-term restorations, and a smooth finish to decrease the tendency to age, discolor or accumulate plaque.
In terms of materials characteristics, is there anything you’re especially excited about both in the near and long term?
Biocompatibility is a major mover in 3D printing, and Formlabs is leading that drive. In the past year, Formlabs has introduced six new resins for biocompatible applications, expanding their use
in dental by nearly double.
THE SMARTER SIPPY
For kids, prolonged use of a sippy cup can lead to cavities. For parents, not using one often means cleaning up spill after infuriating spill. Dentist-entrepreneur Dr. Alene D’Alesio’s invention, the Stick With Me! Stay Put Cup, tackles both issues by helping kids transition to a grownup drinking cup with built-in suction to keep it from spilling. Clever, lighthearted, fun. Problem solved!
—Incisal Edge, SUMMer 2020
DENTAL INNOVATORS HALL OF FAME
INCISAL EDGE IS PROUD TO WELCOME TWO NEW INDUCTEES INTO THIS CELEBRATED GROUP FOR 2021.
RICHARD SASLOW (1932–2020)
CHAIRMAN EMERITUS, HU-FRIEDY
 Chances are, someone in your practice touched a Hu-Friedy instrument today—or, more likely, several of them. That’s due to the drive of Richard Saslow, who purchased the tiny boutique manufacturer in 1959 and built it into an international powerhouse.
Chances are, someone in your practice touched a Hu-Friedy instrument today—or, more likely, several of them. That’s due to the drive of Richard Saslow, who purchased the tiny boutique manufacturer in 1959 and built it into an international powerhouse.
Over the years, Saslow’s leadership established Hu-Friedy as an innovation driver both large and small. Its award-winning Instrument Management System (IMS), developed in concert with Dr. Charles Jerge, changed the way dental practices organize, sterilize, transport and store procedural setups. But it was the decades of constant manufacturing, design refinement and quality obsession championed by Saslow that propelled Hu-Friedy’s success as a world leader in dental instruments and products.
Born just outside Chicago, Saslow attended Evanston High School and Northwestern University before serving in the Army Counterintelligence Corps. He spent his first few years at the head of Hu-Friedy learning the business, but by the 1970s, his unique growth strategies took flight. The company worked closely with dental thought leaders to develop application-specific instruments, then named them after the doctors themselves. It also focused on establishing a presence in dental schools, developing loyalty for its products before future dentists had graduated. All the while, Saslow empowered employees to make important decisions and, above all, focus on the one area of innovation with which he was most obsessed: quality. —Edward Kobesky
DR. ANNE EITING KLAMAR
CHAIR OF THE BOARD OF DIRECTORS, MIDMARK FORMER PRESIDENT AND CEO, 1999–2016
 Stepping intO HER leadership role as a wave of digital technology began transforming health care, Anne Eiting Klamar steered Midmark’s entry into the dental market, as well as its transformation into an R&D-focused developer of comprehensive, highly ergonomic treatment environments.
Stepping intO HER leadership role as a wave of digital technology began transforming health care, Anne Eiting Klamar steered Midmark’s entry into the dental market, as well as its transformation into an R&D-focused developer of comprehensive, highly ergonomic treatment environments.
Dr. Klamar began her career practicing medicine at Family Practice Physicians in Urbana, Ohio, in 1993, and served as director of the Well Child Clinic. She was elected to Midmark’s board of directors that same year and held the position of board secretary before coming on as president in 2000 and being appointed CEO in 2003. She is the fourth generation of the Eiting family to hold a leadership role at Midmark.
Dr. Klamar led the company through an era of growth unprecedented in its history. Midmark’s strategic initiatives—including a series of eight well-timed mergers and acquisitions—helped expand not only its capabilities, but also its physical footprint both domestically and abroad. She transitioned to her current role after celebrating Midmark’s 100th year in 2015. A graduate
of the University of Michigan, she received her M.D. from the Ohio State University and was a graduate of the Owner/President Management program at Harvard. In addition, she’s a committed philanthropist who spurred Midmark’s giving efforts, and a passionate proponent of higher education and community involvement. —E.K.
DENTAL INNOVATORS HALL OF FAME
2019
DR. ESTHER WILKINS
2018
DR. FRANCIS MOUYEN
2017
DR. RAFAEL BOWEN
DAVID SCHICK
2016
DR. RICHARD PELTON AND ERNEST CRANE
DR. GORDON J. CHRISTENSEN
2015
DR. ROBERT MEYER
DR. LUCY HOBBS
2014
DR. JACK DILLENBERG
DR. HOWARD FARRAN
2013
DR. WILLIAM B. DRAGAN
DR. JOHN V. BORDEN
2012
DR. JOSHUA FRIEDMAN
JIM GLIDEWEL
Editor’s Note: Benco Dental, the publisher of Incisal Edge, sells thousands of products, including some that are mentioned in this package. Readers are encouraged to consider multiple sources of information, including those of their colleagues and other publications, prior to making purchase decisions.