Fluoride is good for dentistry, and dentists. Now, for the first time in decades, it’s under attack, driven by the No. 1 most influential person in dentistry this year: Health & Human Services secretary Robert F. Kennedy Jr.
By Mark Caro
“HAVE YOU EVER heard of a thing called fluoridation? Fluoridation of water?”
“Uh, yes, I have heard of that, Jack, yes.”
“Well, do you know what it is?”
“No, no, I don’t know what it is, no.”
“Do you realize that fluoridation is the most monstrously conceived and dangerous Communist plot we have ever had to face?”
That exchange comes from Stanley Kubrick’s legendary 1964 black comedy Dr. Strangelove. The humor comes from absurdity: Fluoride has been used in public water supplies since 1945, and by the time of Strangelove’s release two decades hence, its effectiveness in fighting cavities and tooth decay was widely known.
Yet today, 80 years since its introduction, fluoridation in water is being demonized anew—this time without the laughter. Even before the election, new Health & Human Services Secretary Robert F. Kennedy Jr. was posting that “on January 20, the Trump White House will advise all U.S. water systems to remove fluoride from public water,” adding that “fluoride is an industrial waste associated with arthritis, bone fractures, bone cancer, IQ loss, neurodevelopmental disorders and thyroid disease.” Maybe not a Communist plot—but close.
And while the administration hasn’t adhered to that timetable, Kennedy’s War on Fluoride is officially on. He told the Associated Press in early April that he plans to direct the Centers for Disease Control & Prevention to stop recommending fluoridation of community water supplies. His department announced the same day that it was assembling a task force “to study and make a new recommendation on fluoride.” (Requests from Incisal Edge for interviews with or responses from Kennedy and HHS went unanswered.)
Some states, meanwhile, have taken the cue, and taken action. Utah started banning water fluoridation this spring and forbids local municipalities from overriding its edict. “I’m very, very proud of this state for being the first state to ban it, and I hope many more will,” Kennedy said. Florida then followed suit, with Governor Ron DeSantis terming fluoridation “forced medication.” More states, under the banner of Kennedy’s “Make America Healthy Again” campaign, are expected to follow suit.
Eighty years of community water fluoridation at optimal levels has proven safe and effective at reducing tooth decay and maximizing citizens’ oral health. Utah House Bill 81 ends one of the most equitable, trusted and tested public health strategies in the arsenal of preventive medicine.”
— American Dental Association
This puts America’s dental community at a crossroads. Good dental hygiene is good for dentistry and good for dentists. While a debate about fluoridation is healthy—the need for fluoridation is less urgent in many communities than it was decades ago, given better dental products, many of which contain the mineral—the demonization of fluoride isn’t. Suddenly, one of the pillars of oral health has become highly political.
The American Dental Association has jumped into the fray, swiftly condemning Utah legislators’ “wanton disregard for the oral health and well-being of their constituents” in a statement. “Eighty years of community water fluoridation at optimal levels has proven safe and effective at reducing tooth decay and maximizing citizens’ oral health. [Utah] House Bill 81 ends one of the most equitable, trusted and tested public health strategies in the arsenal of preventive medicine.”
The American Association for Dental, Oral and Craniofacial Research (AADOCR) also released a statement backing the efficacy and safety of fluoride in public water supplies. “Community water fluoridation is a safe method of delivering fluoride on a population level,” it reads. “There have been numerous systematic reviews on claims of the potential adverse health effects of water fluoridation. None has concluded that there is a significant or consistent association between water fluoridation and the outcomes examined, including neurologic conditions, cancer and osteoporosis.”
Dr. Bill Maas, the Centers for Disease Control’s former director of oral health and now a Maryland-based dental public health consultant, expressed dismay that Kennedy and others are blaming fluoridated water for an array of serious health problems despite much research to the contrary. “Somebody referred to these as ‘zombie claims’—they come back from the dead,” Maas says.
“We thought we put these questions to sleep.”
They are now wide awake.

When a similar issue arose in Bauxite, Arkansas, McKay and another researcher published a paper that prompted a chemist, H.V. Churchill of Alcoa, to conduct tests on the water. They revealed a high level of fluoride present. Churchill reported his findings to McKay in 1931, and samples collected in the other towns previously afflicted by brown teeth also showed high fluoride levels. After 30 years, the mystery had been solved.
But although high levels of fluoride were deemed responsible for fluorosis, the term for such tooth-enamel discoloration, McKay’s studies also indicated that the afflicted teeth were resistant to decay. Further research on this subject, led by H. Trendley Dean, head of the NIH’s Dental Hygiene Unit, found that low levels of fluoride in drinking water did not cause fluorosis yet protected teeth against decay.
This theory was put to the test when, in 1945, Grand Rapids, Michigan, became the world’s first city to add fluoride to its drinking water. Researchers monitored tooth decay in almost 30,000 schoolchildren, and 11 years into a 15-year project, Dean announced that incidence of tooth decay had dropped by more than 60 percent among children born after fluoridation began.
“This finding, considering the thousands of participants in the study, amounted to a giant scientific breakthrough that promised to revolutionize dental care, making tooth decay for the first time in history a preventable disease for most people,” the NIDCR history states.
Fluoridation has since become standard in the U.S. According to the CDC’s most recent Water Fluoridation Statistics, from 2022, about 289 million people among the total U.S. population of some 333 million were on community water systems, and roughly 209 million of those were on fluoridated drinking water systems. That translates to 62.8 percent of the U.S. population receiving fluoridated water and 72.3 percent of those on community water systems receiving fluoridated water.
When the CDC touted the twentieth century’s “Ten Great Public Health Achievements” in the U.S., fluoridation of drinking water was listed alongside vaccination (another Kennedy bugbear), motor-vehicle safety, safer workplaces, control of infectious diseases, decline in deaths from coronary heart disease and stroke, safer and healthier foods, healthier mothers and babies, family planning and recognition of tobacco use as a health hazard.
Researchers monitored tooth decay in almost 30,000 schoolchildren, and 11 years into a 15-year project, they announced that tooth decay had dropped by more than 60 percent among children born after fluoridation began.
Although the CDC says it “does not mandate community water fluoridation,” it considers it to be “a cornerstone strategy for prevention of cavities in the U.S. It is a practical, cost-effective and equitable way for communities to improve their residents’ oral health regardless of age, education or income. . . . Drinking fluoridated water keeps teeth strong and reduces cavities by about 25 percent in children and adults. This results in less mouth pain, fewer fillings or teeth pulled and fewer missed days of work and school.”
The CDC further reports that “communities of 1,000 or more people see an average estimated return on investment (ROI) of $20 for every $1 spent on water fluoridation. The ROI for community water fluoridation increases as the community size increases, but even small communities save money. Communities served by fluoridated water save an average of $32 per person a year by avoiding treatment for cavities.”
“
Public water fluoridation in other parts of the world varies. Most of Australia’s drinking water is fluoridated, as is Canada’s, though some municipalities have banned it. Calgary, Alberta, removed fluoride from its water supply in 2011, but after a decade of increased dental problems, residents voted to reinstate it; its government announced it would be reintroduced into drinking water in the second quarter of this year.
Communities served by fluoridated water save an average of $32 per person a year by avoiding treatment for cavities.”
—CDC
Most of Ireland’s water is fluoridated. Most of the U.K.’s is not; fluoride is added to about 10 percent of those countries’ drinking water, according to a December 2024 report from the Parliamentary Office of Science and Technology, though fluoride also naturally occurs at low levels in some English water supplies. Much of Europe’s water is not fluoridated, yet countries such as Germany, France, Switzerland and the Czech Republic offer fluoridated salt to compensate.
Despite Dr. Strangelove, the U.S. military has actively supported water fluoridation, including on overseas bases. In a memo dated March 18, 2013, John Conger, then the acting deputy undersecretary of defense, called on the secretaries of the Army, Navy and Air Force to ensure that fluoridated water was provided at all Department of Defense installations in the U.S. and abroad. “The Assistant Secretary of Defense for Health Affairs has determined that providing optimally fluoridated water at DoD installations helps to improve and sustain the military readiness and health of military personnel,” the memo said, citing a 2011 ASD(HA) memorandum on the subject. “[T]he ASD(HA) identifies dental decay as a significant reason for military personnel to be classified as nondeployable and recommends optimizing fluoridation in DoD potable water treatment systems.”
The CDC’s Dr. Maas noted that Trump’s first administration made no effort to roll back these requirements. The concept of fluoridation indeed seemed to be settled science.
SO WHAT’S DIFFERENT NOW? One word: Covid, which has made large swaths of society far more skeptical about government mandates and universal health policies.
You could see some of that play out around fluoridation 60 years ago. The far-right John Birch Society actively opposed and campaigned against it in a 1964 referendum battle in Wichita, Kansas. As the Wichita Eagle noted in 2014: “During that debate, some opponents labeled the pro-fluoridation forces as ‘tools of the Communists’ and one anti-fluoride publication asked: ‘Shall we give the Communists the machinery and the materials to destroy us by simply opening a valve in our water supply?’ ”
“The ASD(HA) identifies dental decay as a significant reason for military personnel to be classified as nondeployable and recommends optimizing fluoridation in DoD potable water treatment systems.”
Water fluoridation in Wichita was voted down in 1964 and 1978. It was back on the ballot in 2014 after a coalition of Wichita dentists and other medical professionals sponsored an initiative to add the mineral to the community water. The debate was fierce, and 59 percent of voters rejected it.
Then, as now, a key anti-fluoride argument objected to the government’s supposed incursion into people’s bodily autonomy. “I’m a very strong believer that the government has absolutely no right to put a medication in my body that I don’t want, and in fact that I know is going to cause trouble with multiple organs in my body and probably does no good or very little good for my teeth,” the late Republican activist Mark Gietzen, who campaigned against fluoride, told the Wichita Eagle in 2014.

“There’s a libertarian point of view that we should have choice on the medications that are delivered to us,” he adds. “I agree with that to a point, but there are so many people who don’t have choice, and that’s where public health fills those gaps.”
Dr. Riggs jumped into the fluoride debate when, in 1989, the New England Journal of Medicine published her letter about the lack of fluoride in bottled water. She wrote that she and her colleagues had a lab analyze 12 popular bottled water brands, and only one, Perrier Naturally Sparkling Mineral Water, contained the recommended amount of fluoride.
She saw this finding as a way to warn people against reliance upon bottled water for drinking, but the bottled water industry trumpeted that her study showed that its products “are pure and healthy,” she says. “I was like, ‘What?’ It let them take over the narrative. So I had a very early sense and experience of how tenuous the fluoride debate is.”
It’s probably no coincidence that the anti-fluoride campaign has heated up amid the backlash to various government actions during the pandemic. “The bottom line is after Covid there is this concern about government mandating all these interventions,” says Dr. Jay Kumar, California’s former state dental director.
Dr. Scott Tomar, a public health dentist and oral epidemiologist at the University of Illinois–Chicago, agrees. “I don’t know if some of the distrust is a holdover of some of the angst around Covid shutdowns, but clearly there is something going on where the public is questioning the safety and efficacy of things that have been around for decades with strong track records of effectiveness and safety,” he says, citing the parallel campaign against the measles vaccine and subsequent measles outbreaks.
Dr. Kumar (right) has studied fluoride since 1979, when he was doing a public health residency in New York and investigated what was turning children’s teeth yellow on a Native American reservation. Some thought the cause was water fluoridation, but it turned out to be the tetracycline being taken by the children.

He was also a member of the National Academies of Sciences’ Committee on Fluoride in Drinking Water, which produced an extensive review of the Environmental Protection Agency’s standards in 2006. The committee’s report recommended that the EPA’s maximum allowed fluoride level should be lowered from what then was 4 milligrams per liter. Those relatively high levels were found to naturally occur in some water sources; the level of fluoride being added to community water supplies was 0.7 to 1.2 mg/L. In 2011, the EPA and HHS recommended that fluoride be added to water at the lower end of that scale: 0.7 mg/L.
Dr. Maas noted that when researchers studied a possible connection between fluoride and bone cancer after the 2006 report, samples were collected from children undergoing bone surgery, and the answer came back that fluoride was not a factor.
Current anti-fluoride campaigners have asserted a correlation between fluoridated water and low IQ scores, but a January 2025 Journal of the American Medical Association analysis of 74 studies on the subject—most conducted in China—found that 52 of them “were rated high risk of bias.” Those studies also involved fluoride levels significantly higher than what is allowed in the U.S. An Australian study published in Sage Journals in December 2024 found “consistent scientific evidence that early-life exposure to fluoride was not negatively associated with cognitive neurodevelopment. The findings, in combination with the current body of knowledge, provide assurance that the currently practiced [fluoridation] programs are both effective and safe for young children.”
Says Dr. Kumar: “There is no evidence to say fluoride causes IQ loss at levels that we use in the U.S.”
At the same time, numerous studies show that in places that eliminated fluoridated water, cavities and tooth decay soon became apparent. “It is clear from studies in Calgary; Juneau, Alaska; and Israel that adverse effects can be seen in young children within a few years,” Dr. Maas says. “However, based on our understanding of how [community water fluoridation] works, many people at all life stages will have increased decay. It simply takes longer to see those results in permanent teeth, and it is very difficult to study decay rates in adults because they have lived many different places and because so much restorative care is replacement of fillings placed to address decay earlier in their lives. People of all ages will suffer. We simply won’t know how much until it is too late.”
The Israel example is instructive in another way, he adds. “Some say we don’t need fluoride in water; we need a better health care system.” Yet although Israel provides widespread oral health care without the financial barriers present in the U.S., residents’ oral health still suffered once fluoridation ended. “What Israel showed is giving people access to care didn’t replace the loss they suffered from removing fluoride from water.”
One of Dr. Kumar’s frustrations is that communities that ban fluoride in water “never come up with an alternative treatment.” Tooth decay, after all, can lead to plastic-based or mercury fillings. “I don’t know whether [Kennedy] knows that there are concerns about plastic and mercury as well,” he says. Then there are the X-rays and anesthesia that may accompany oral health procedures. “All those should be weighed against any concerns about fluoride in community water supplies. I don’t know whether they’re thinking along those lines at all.”
There is no evidence to say fluoride causes IQ loss at levels that we use in the U.S.”
—Dr. Jay Kumar
Dr. Maas also laments the lack of apparent big-picture health strategies amid the attacks on fluoridation. For instance, those who think fluoride is harmful might address communities whose water supplies contain higher than optimal levels of fluoride. “If they really believed in people’s health, they’d say, ‘Let’s do something for people with naturally high levels of fluoride in their water,’ ” he says. “Nobody’s doing that.”
He was also puzzled by the elimination in April of the CDC’s 20-person Division of Oral Health among 10,000 jobs that were axed in the Department of Health & Human Services. The division had leveraged its small size by working with all state health departments, he says. “The Division of Oral Health assumed a responsibility to understand the science base about water fluoridation and other public health methods to prevent oral diseases,” says Dr. Maas, who was the division’s director for ten years. “That’s what our job was. Do you think it’s important that there be a government agency that knows the latest science and community-based methods on how to prevent oral diseases?”
DR. MADISON DAY, a Salt Lake City–based dentist, says she was experiencing repercussions of the Utah law in her practice before it even took effect. “My patient base in Salt Lake is very nervous with the fluoride being taken out of the water,” she says. “Every single day I have three or four patients ask me for recommendations, if there’s anything they can do for their kids or grandkids to try to prevent cavities.”

Previously, the UDA provided links encouraging its members to contact legislators to oppose the anti-fluoride bill, which she did. But the governor signed it anyway. “I was really sad and worried,” she says. “I have a baby now. The highest-risk population is little kids, because it’s not like I can have my baby swish with fluoride rinse and spit it out. I’m worried about my patients too.”
She adds that she has seen the problems of unfluoridated water firsthand. “In dental school I did a trip to southern Utah. All my patients down there had well water, and they all had lots of cavities.”

Her office is focusing on kids, recommending they get fluoride prescriptions from their dentist or pediatrician. The legislation lets people get fluoride directly from pharmacists as well, which she hopes will remove some barriers for care.
All the attention community water fluoridation has garnered is allowing us to speak as to why it is important: better oral health.”
—Dr. Brett Kessler
“Something I appreciate about all the talk about fluoride now is that we’re able to talk about oral health in general,” Dr. Bank says, noting that “1.6 million people in Utah will now be without fluoride in their water, but that’s two counties in one city. The rest of the state hasn’t had fluoridated water anyway. So this is an opportunity for us to talk about oral health, the benefits of fluoride and the risks of fluoride, so people who are concerned have a chance to be educated as well.”
The ADA, which sent an email to members in mid-May noting $20 million in budget reductions in addition to $9 million in recent cuts, has finite resources to pursue its existing agenda in addition to relitigating water fluoridation. But Dr. Kessler says the Trump administration’s actions have not put the organization in an either/or position.
“Certainly, it’s disheartening to have to fight community water fluoridation in the wake of 80 years of credible research, but it in no way distracts us from focusing on other priority issues,” he says. “In fact, just the opposite. All the attention community water fluoridation has garnered is allowing us to speak as to why it is important: better oral health.”
He senses that most dentists support the organization’s pro-fluoridation stance, even though many are Republicans. “I think dentists in general lean more to the right [politically], but I feel like most of my colleagues and most of the population in America is very centered,” he says. “For the most part, I’m getting general support for science, which is what we at the ADA believe in.”
The American Dental Political Action Committee supported three incumbent House members who were reelected in November: Dr. Brian Babin of Texas, Dr. Mike Simpson of Idaho and Dr. Jeff
Van Drew of New Jersey. All are Republicans. Calls and emails to their press representatives were not returned.
“All of our people in Congress are Republicans,” Dr. Kessler says. “All the dentists are. I haven’t been following their statements; I’m just following ours. We love our members of Congress, and they do a lot for us.”
The ADA no longer backs Arizona Rep. Dr. Paul Gosar, who before joining Congress in 2013 was a practicing dentist for 25 years and was inducted into the Arizona Dental Association Hall of Fame. As a House member, Dr. Gosar objected to the certification of Joe Biden’s 2020 election, praised the January 6 rioters and was censured for posting a clip showing a video game version of himself
killing a video game version of Rep. Alexandria Ocasio-Cortez and attacking a video game Biden. Calls and emails to Dr. Gosar’s office for comment also went unreturned.
In mid-April, Dr. Kessler posted this message on his social media accounts:

CWF is a mitigation strategy in place to reduce rampant decay—especially in low-income children. If it goes away, real science says that cavity rates will increase by over 25%. This means we will be dooming our children to a lifetime of dental problems that otherwise could have been avoided by maintaining the CWF.
There are little to no side effects or adverse effects of CWF at the current recommended levels. This is from over 70 years of research in the field.
It’s time to shift the focus on the ROOT cause of cavities, Mr. Kennedy—SUGAR and ULTRAPROCESSED FOOD. Please quit vilifying dental professionals for trying to mitigate the problem caused by the food industry.
We at the @Americandentalassociation look forward to working with you on this.
@bikodds
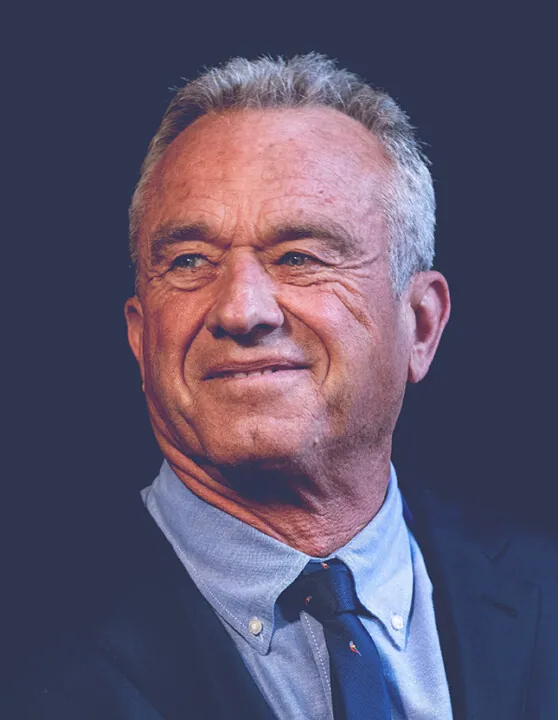
Says Dr. Kumar: “There are always dentists who have opposed water fluoridation, but the overwhelming majority of dentists—Republicans, Democrats or independents—go by what the science says.”
Dr. Day noted that some people have joked that she’ll get more work once fluoride is out of Utah’s water. But that’s not what she wants. “Good dentists don’t want to have to do a lot of fillings,” she says. “They want healthy patients.”